More than 96 million adults in the U.S. have prediabetes-and 80% don’t even know it. That’s not just a number. It’s your neighbor, your coworker, maybe even you. The good news? You don’t need drugs or surgery to turn things around. What you do need is a simple, science-backed way of eating that keeps your blood sugar steady, your energy up, and your risk of type 2 diabetes way down.
Why Fiber Is Your Secret Weapon
Fiber doesn’t just help you feel full. It slows down how fast sugar enters your bloodstream. That’s huge when you’re trying to avoid spikes and crashes. The goal? 25 to 38 grams a day, depending on your age and gender. Most people get less than half that. Start with what’s already on your plate: veggies. One cup of broccoli gives you 5 grams of fiber. Spinach, peppers, zucchini-each serving adds 3 to 5 grams. That’s easy to stack. Fill half your plate with non-starchy vegetables at every meal. It’s not a suggestion; it’s the baseline. Switch your grains. If you’re eating white bread, white rice, or regular pasta, you’re missing out. The American Diabetes Association says at least half your grains should be whole. Swap white rice for quinoa (GI 53), or try barley instead of white bread. Steel-cut oats aren’t just a trend-they’re a game-changer. One bowl gives you 4 grams of fiber and keeps your morning glucose stable, unlike instant oatmeal, which spikes it fast. Legumes are another powerhouse. Lentils, chickpeas, black beans-they’re packed with fiber and protein. Add a cup to your salad or soup. That’s 15 grams of fiber right there. And you don’t need to eat them every day. Just a few times a week cuts your diabetes risk by 23% for every extra 10 grams of fiber you get, according to a 2021 study in the American Journal of Clinical Nutrition.Protein Isn’t Just for Muscles
Protein doesn’t raise blood sugar. But more than that-it slows down the sugar from everything else you eat. Pair a banana with peanut butter. Add eggs to your toast. Have Greek yogurt with berries. These combos keep glucose from shooting up. The ADA recommends getting 15-20% of your daily calories from protein. That’s about 2-3 palm-sized portions a day. But not all protein is equal. Lean meats, fish, eggs, and tofu are ideal. Red meat? Limit it. A 2020 study in Diabetologia found that eating just 100 grams of red meat a day-about the size of a deck of cards-raises your diabetes risk by 20%. Plant proteins are doubly helpful. Lentils, beans, edamame, and tempeh give you fiber AND protein in one package. A bowl of lentil soup with spinach and tomatoes isn’t just comforting-it’s a diabetes-fighting meal. Timing matters too. A small apple with 2 tablespoons of natural peanut butter at 3 p.m. can stop a sugar crash and prevent overeating later. Same with a handful of almonds with your afternoon fruit. You’re not snacking-you’re stabilizing.Glycemic Index: It’s Not Magic, But It’s Real
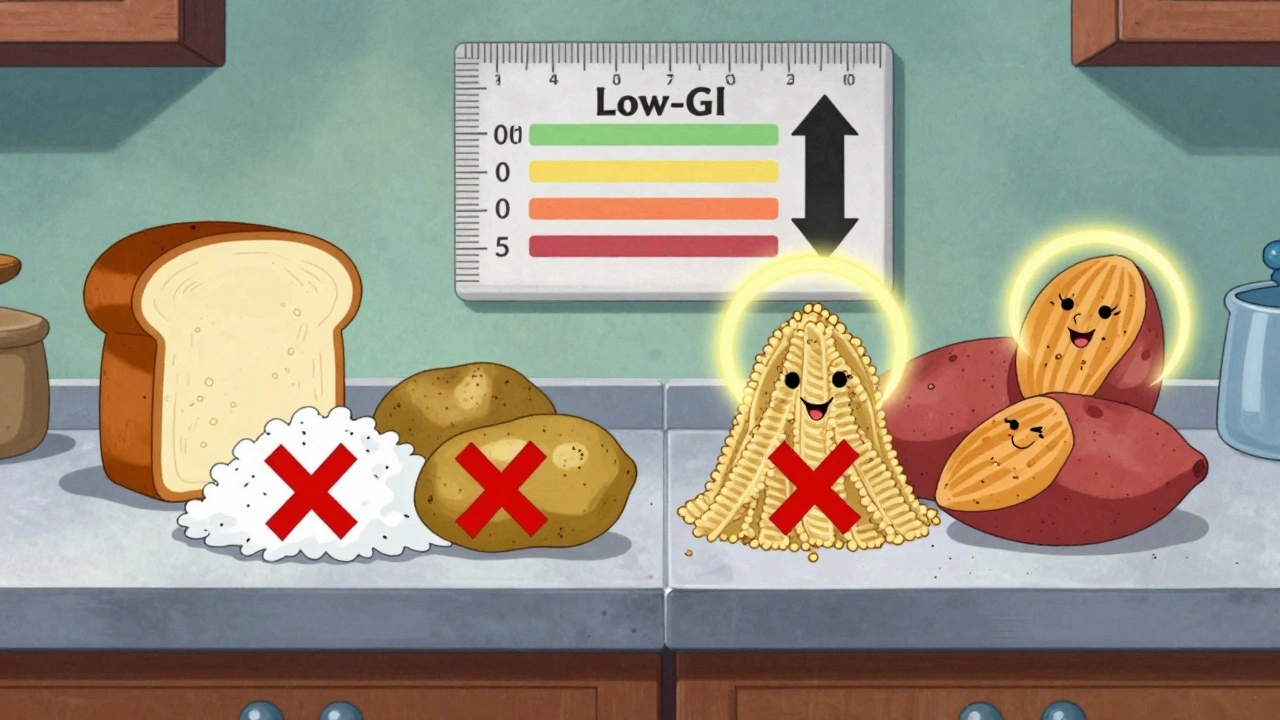
The glycemic index (GI) tells you how fast a food turns into sugar in your blood. High-GI foods (70+) spike glucose fast. Low-GI foods (55 or below) roll it in slowly. Here’s what to avoid: white bread (GI 75), white rice (GI 73), and potatoes (GI 85). These are staples in many diets-but they’re the enemy of blood sugar control. Swap them out:- White rice → Brown rice (GI 50) or quinoa (GI 53)
- Potatoes → Sweet potatoes (GI 44)
- Instant oatmeal → Steel-cut oats (GI 55)
- White pasta → Whole wheat or chickpea pasta (GI 40-45)
The Mediterranean Diet Works-But You Don’t Have to Be Italian
The Mediterranean diet isn’t about olives and feta alone. It’s about plants first, healthy fats second, and protein third. Think: vegetables, beans, nuts, fish, olive oil, and occasional chicken or eggs. Red meat? Rare. Sugar? Almost never. It’s not a diet you follow for a month. It’s a way of eating that lasts. Studies show it improves blood sugar control and lowers heart disease risk-both critical for prediabetes. You don’t need to cook like a chef. Start small:- Use olive oil instead of butter
- Have fish twice a week
- Snack on walnuts or almonds
- Make a big salad with beans and vinaigrette for lunch
What to Avoid (Beyond Sugar)
It’s not just about cutting out candy. Some hidden traps are worse:- Flavored yogurts-often have 20+ grams of sugar
- Granola bars-look like healthy snacks, but are sugar bombs
- Low-fat products with added sugar to make them taste good
- Artificial sweeteners-some studies link them to insulin resistance, even if they don’t raise blood sugar
- Trans fats and saturated fats from butter, cream, coconut oil, and hard margarines

Real People, Real Results
One user on Diabetes Daily switched from instant oatmeal to steel-cut oats and saw his morning blood sugar drop by 30 points. Another on Reddit paired fruit with Greek yogurt and kept his post-meal glucose under 140-down from 180. But it’s not easy. In a 2022 survey, 42% of people struggled to eat enough veggies every day. Two-thirds had trouble with portion control. That’s normal. Change is hard. Use the plate method: half your plate non-starchy veggies, one-quarter lean protein, one-quarter whole grains or starchy veggies. No measuring cups needed. Just eyeball it. People who use this method stick to it 27% longer.It’s Not About Perfection
You don’t need to eat perfectly every day. You need to make better choices most days. One meal won’t make or break you. But your habits over weeks and months will. The Diabetes Prevention Program proved it: lifestyle changes cut diabetes risk by 58% over three years. That’s better than any drug. And you don’t need a gym membership or a nutritionist. You need to eat more fiber, more protein, and more low-GI foods-and less of the rest. Start with one change this week. Swap white rice for quinoa. Add a cup of beans to your soup. Eat an apple with peanut butter instead of a granola bar. Small steps. Big results.What’s Next?
If you’ve made these changes for a few weeks and your energy’s better, your cravings are quieter, and your blood sugar readings are steadier-you’re on the right path. Keep going. If you’re still unsure where to start, talk to your doctor about a structured program. Medicare and many insurers cover the National Diabetes Prevention Program. It’s free or low-cost. It’s proven. And it’s designed for people exactly like you.This isn’t about becoming someone else. It’s about becoming healthier than you were yesterday.
Can I eat fruit if I have prediabetes?
Yes-but choose wisely. Berries, apples, pears, kiwi, and citrus fruits are low in sugar and high in fiber. Stick to one cup per serving. Pair them with protein like Greek yogurt, nuts, or cheese to slow sugar absorption. Avoid fruit juices and dried fruit-they’re concentrated sugar with no fiber.
How much protein should I eat daily with prediabetes?
Aim for 15-20% of your daily calories from protein. For most adults, that’s about 2-3 palm-sized portions of lean meat, fish, eggs, tofu, or legumes per day. Plant-based proteins like lentils and beans are ideal because they also provide fiber. Avoid processed meats and limit red meat to once a week or less.
Is the keto diet good for prediabetes?
Keto can lower blood sugar in the short term, but it’s not sustainable for most people-and it may raise LDL cholesterol if it’s high in saturated fat. Long-term studies show no clear advantage over balanced, fiber-rich diets like the Mediterranean pattern. Focus on whole foods, not extreme restrictions. If you try keto, monitor your cholesterol and talk to your doctor.
Do I need to count calories with prediabetes?
Not necessarily. What matters more is what you eat, not how many calories. Prioritize fiber, protein, and low-GI foods, and you’ll naturally eat less without feeling hungry. If you’re trying to lose weight, aim for 5-10% of your starting weight-that’s enough to cut diabetes risk by half. Use portion control and the plate method instead of calorie counters.
Can I still drink alcohol with prediabetes?
Moderation is key. One drink a day for women, two for men. Choose dry wine, light beer, or spirits with soda water and lime. Avoid sugary mixers, sweet wines, and cocktails. Alcohol can cause blood sugar to drop later, especially if you’re on medication. Always eat food when you drink.
How long does it take to reverse prediabetes?
Many people see improvements in blood sugar within 3-6 months of consistent lifestyle changes. Reversing prediabetes-meaning returning to normal glucose levels-often takes 6-12 months. The key is consistency, not speed. Even small, steady improvements reduce your risk of type 2 diabetes by up to 58%.