When you get sick - fever, sore throat, cough, body aches - it’s natural to wonder: is this bacterial or viral? The answer changes everything. Taking the wrong treatment doesn’t just waste time; it can make things worse. And you’re not alone in being confused. Nearly 7 out of 10 people don’t know that antibiotics don’t work on viruses. That misunderstanding is fueling a global health crisis.
What’s Really Going On Inside Your Body?
Bacteria and viruses are not the same. They don’t just look different - they behave completely differently. Bacteria are single-celled living organisms. They can survive on their own, in soil, water, or on your skin. They reproduce by splitting in half - sometimes every 20 minutes. That’s why a simple cut can turn into a serious infection if bacteria get in.
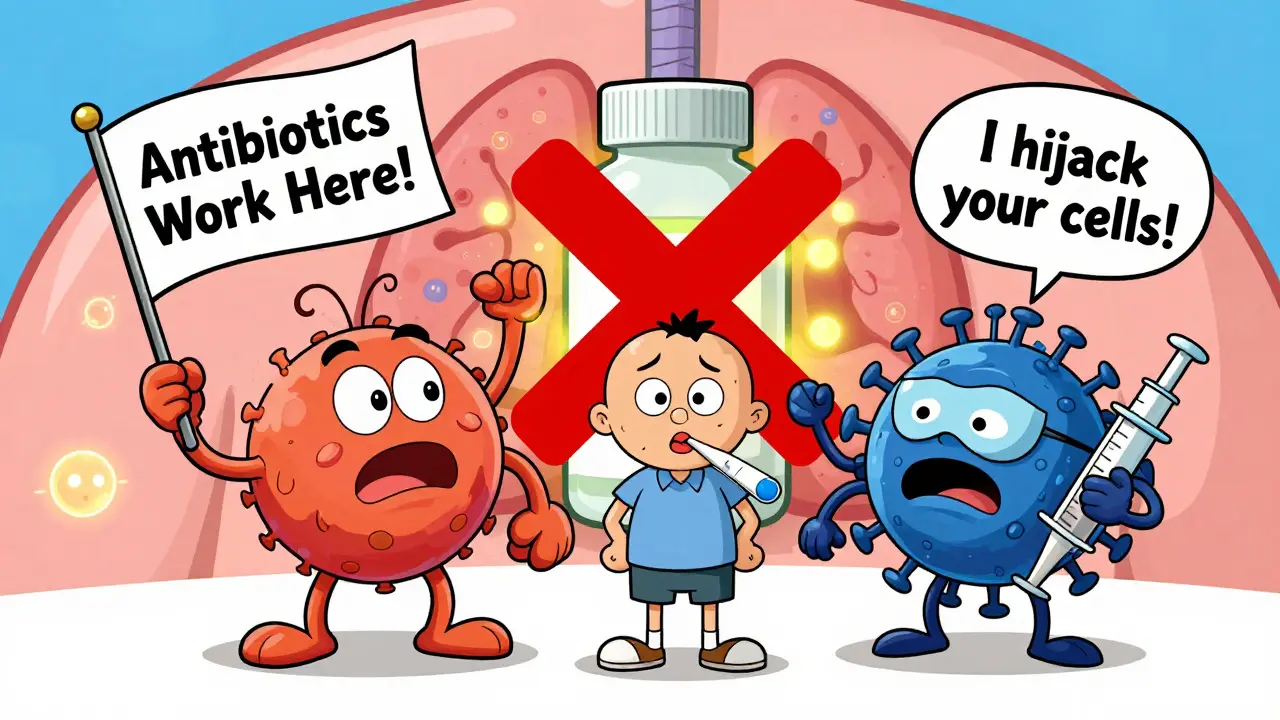
Viruses are not alive in the way we think of life. They’re just genetic material - DNA or RNA - wrapped in a protein shell. They can’t reproduce on their own. They have to sneak into your cells and take over. Once inside, they force your body to make copies of them, which then burst out and infect more cells. That’s why you feel awful - your body is fighting back against a hijacking operation.
Size matters too. The biggest viruses are about 300 nanometers across. The smallest bacteria are around 200 nanometers. That’s why you can’t see viruses under a regular microscope. You need an electron microscope. This tiny size lets them slip through barriers bacteria can’t.
Common Infections: What’s Bacterial? What’s Viral?
Here’s what you’re likely to run into:
- Bacterial: Strep throat (caused by Group A streptococcus), urinary tract infections (UTIs), tuberculosis, and some sinus infections. Strep throat alone affects over 600 million people every year globally. UTIs lead to over 8 million doctor visits in the U.S. each year.
- Viral: The common cold (usually rhinovirus), flu (influenza), chickenpox (varicella-zoster), COVID-19 (SARS-CoV-2), and most cases of bronchitis and sinusitis. The flu hits 9 to 41 million Americans annually. Before vaccines, chickenpox had 4 million cases a year worldwide.
One big surprise? About 85% of acute bronchitis cases and 70% of sinus infections are viral - not bacterial. But most people still ask for antibiotics. That’s not just unnecessary - it’s dangerous.
How Symptoms Can Trick You
Both types of infections can give you fever, cough, sore throat, and fatigue. So how do you tell them apart? Here’s what doctors look for:
- Bacterial infections often come with higher fevers - above 101°F (38.3°C). Symptoms that last more than 10 to 14 days, or that get better then suddenly get worse, are a red flag. Think: you felt okay for five days, then your cough came back hard. That could mean a secondary bacterial infection.
- Viral infections usually start with a runny nose, mild fever (under 100.4°F), body aches, and a cough. Most improve within 7 to 10 days. The common cold? It’s gone in about a week.
But here’s the catch: viral infections can lead to bacterial ones. About half of people hospitalized with severe viral pneumonia - like from COVID-19 - end up with a bacterial infection on top of it. That’s why antibiotics are sometimes needed in hospitals - not to treat the virus, but to stop the secondary bacterial infection.
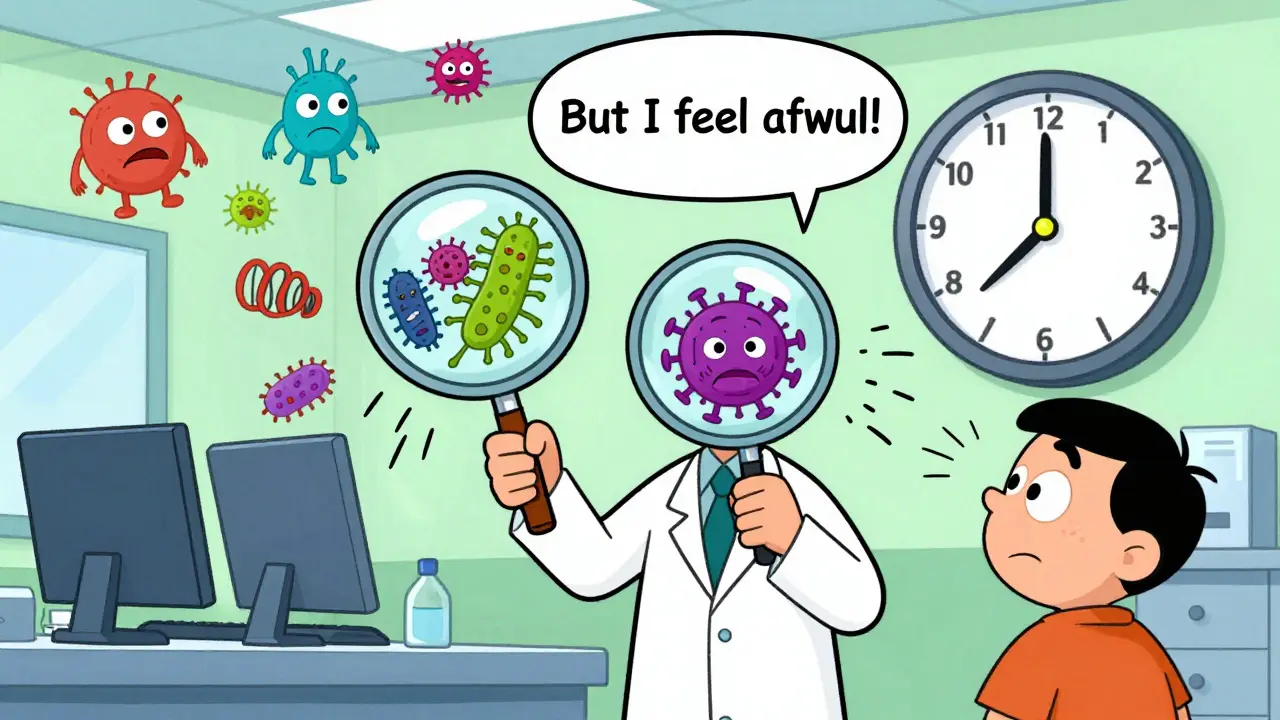
Testing: The Only Way to Know for Sure
Guessing based on symptoms isn’t enough. Doctors use tests to be sure.
- Rapid strep test: Swabs the throat. Detects Group A strep with 95% accuracy. Takes 10 minutes.
- Throat culture: The gold standard. Takes a couple days but is 98% accurate.
- PCR test (for viruses): Used for flu, COVID-19, RSV. Detects viral genetic material. 90-95% accurate if done within the first 72 hours.
- FebriDx: A newer test approved in 2020. Measures two biomarkers - CRP (inflammation) and MxA (viral response). Gives results in 10 minutes with 94% sensitivity for viral infections. It’s helping doctors avoid unnecessary antibiotics.
For strep throat, doctors use the Centor Criteria: fever, no cough, swollen lymph nodes, and white patches on tonsils. If you have 3 or more of these, you have a 50-55% chance of strep - enough to justify testing.
Why Antibiotics Don’t Work on Viruses
Antibiotics attack bacteria. They break down their cell walls, stop them from making proteins, or block their DNA replication. Viruses don’t have any of those structures. They’re not cells. They’re just genetic code inside a protein shell. Antibiotics are like a wrecking ball aimed at a house - useless against a key.
Using antibiotics for viruses doesn’t just do nothing - it harms you. It kills off good bacteria in your gut, which can lead to diarrhea, yeast infections, or worse - Clostridioides difficile (C. diff). In the U.S., C. diff causes over 220,000 infections and 12,800 deaths every year.
And it’s not just you. Every time you take an unnecessary antibiotic, you’re helping bacteria become resistant. The World Health Organization calls antibiotic resistance one of the top 10 global health threats. In 2019, drug-resistant infections killed 1.27 million people worldwide. By 2050, that could hit 10 million - more than cancer.

Treatment: What Actually Helps
For bacterial infections:
- Antibiotics are the go-to. Penicillin for strep throat (10-day course), ciprofloxacin for UTIs, isoniazid for tuberculosis.
- Finish the full course. Even if you feel better in 3 days. Stopping early lets tough bacteria survive and multiply.
For viral infections:
- Most need no medicine. Rest, fluids, and fever reducers like acetaminophen or ibuprofen are enough.
- Some have antivirals - but timing is everything. Oseltamivir (Tamiflu) for flu must be taken within 48 hours of symptoms to shorten illness by 1-2 days. Remdesivir for severe COVID-19 works best early in hospital settings.
- For chickenpox or shingles, acyclovir helps reduce severity if started early.
And here’s something surprising: the CDC says antibiotics should never be prescribed for viral upper respiratory infections. Yet, in the U.S., doctors write 47 million unnecessary antibiotic prescriptions every year. That’s about 30% of all antibiotic prescriptions for colds and flu.
The Bigger Picture: Cost, Risk, and Future Solutions
It’s not just about your health. Misuse of antibiotics costs the U.S. healthcare system $1.1 billion a year. Viral respiratory illnesses? They cost $45 billion annually in medical bills and lost workdays. Kids miss 22 million school days. Parents miss 20 million workdays.
But there’s hope. Researchers are working on new tools:
- Narrow-spectrum antibiotics: Target only specific bacteria, sparing your good microbes.
- Phage therapy: Uses viruses that infect only bacteria. In recent European trials, it’s shown 85% effectiveness against resistant infections.
- Universal coronavirus vaccines: In Phase III trials as of 2024. Could prevent future pandemics.
The WHO’s Global Antimicrobial Resistance Surveillance System found resistance to first-line antibiotics jumped from 5.8% in 2017 to 17.3% in 2023. That’s a 200% increase in just six years.
What You Should Do
Here’s what to remember:
- Don’t ask for antibiotics for a cold or the flu. They won’t help.
- If you’re sick for more than 10 days, or symptoms get worse after improving, see a doctor. You might have a bacterial infection.
- Get tested if your doctor suspects strep or flu. Don’t rely on symptoms alone.
- Take antibiotics exactly as prescribed. Never save leftovers. Never share them.
- Wash your hands. Get vaccinated. Flu shots, MMR, and COVID boosters reduce spread and protect others.
The line between bacterial and viral isn’t always clear - but the treatment difference is absolute. Your choices matter. Not just for you. For everyone.
Can antibiotics treat a viral infection like the flu?
No. Antibiotics target bacteria, not viruses. The flu is caused by influenza viruses, so antibiotics won’t shorten the illness or reduce symptoms. Taking them anyway can cause side effects like diarrhea or yeast infections and increase the risk of antibiotic-resistant bacteria. Antiviral medications like oseltamivir (Tamiflu) are the only drugs that can help with flu - and only if taken within 48 hours of symptoms starting.
Why do doctors sometimes prescribe antibiotics for colds or sore throats?
Sometimes, it’s because they’re unsure. Many colds and sore throats are viral, but symptoms overlap with bacterial infections like strep. In busy clinics, doctors may prescribe antibiotics to satisfy patient demand or avoid follow-up visits. But guidelines are clear: antibiotics should only be used when testing confirms a bacterial cause. The Centor Criteria and rapid strep tests help reduce unnecessary prescriptions.
Is a high fever always a sign of a bacterial infection?
Not always. While bacterial infections often cause higher fevers (above 101°F), some viral infections - like influenza or COVID-19 - can also spike your temperature. Fever alone isn’t enough to tell the difference. Doctors look at the whole picture: how long symptoms last, whether they improve then worsen, presence of cough, and test results. A fever of 103°F could be viral - and doesn’t automatically mean you need antibiotics.
How long should symptoms last before I worry about a bacterial infection?
If your symptoms last more than 10 to 14 days without improvement, or if you start feeling better then suddenly get worse (like a cough returning with thicker mucus or new fever), that’s a red flag for a secondary bacterial infection. For example, a viral cold that turns into bacterial sinusitis or pneumonia. In these cases, antibiotics may be needed. But if symptoms are improving by day 7, you likely have a virus.
Can I prevent bacterial and viral infections?
Yes. Handwashing, avoiding close contact with sick people, and staying up to date on vaccines are your best defenses. Flu, COVID-19, and pneumococcal vaccines prevent many viral and bacterial infections. The pneumococcal vaccine protects against bacterial pneumonia. The MMR vaccine prevents measles - which can lead to secondary bacterial infections. Prevention is far more effective than treatment.