
When people start using cannabis - whether for pain, anxiety, or sleep - they often don’t realize how it might be changing the way their other medications work. It’s not just about feeling more relaxed or drowsy. Cannabis, especially CBD and THC, can seriously affect how your body processes common drugs like blood thinners, seizure medications, and even antidepressants. And the consequences? They can be dangerous - even life-threatening.
How Cannabis Changes How Your Body Handles Medications
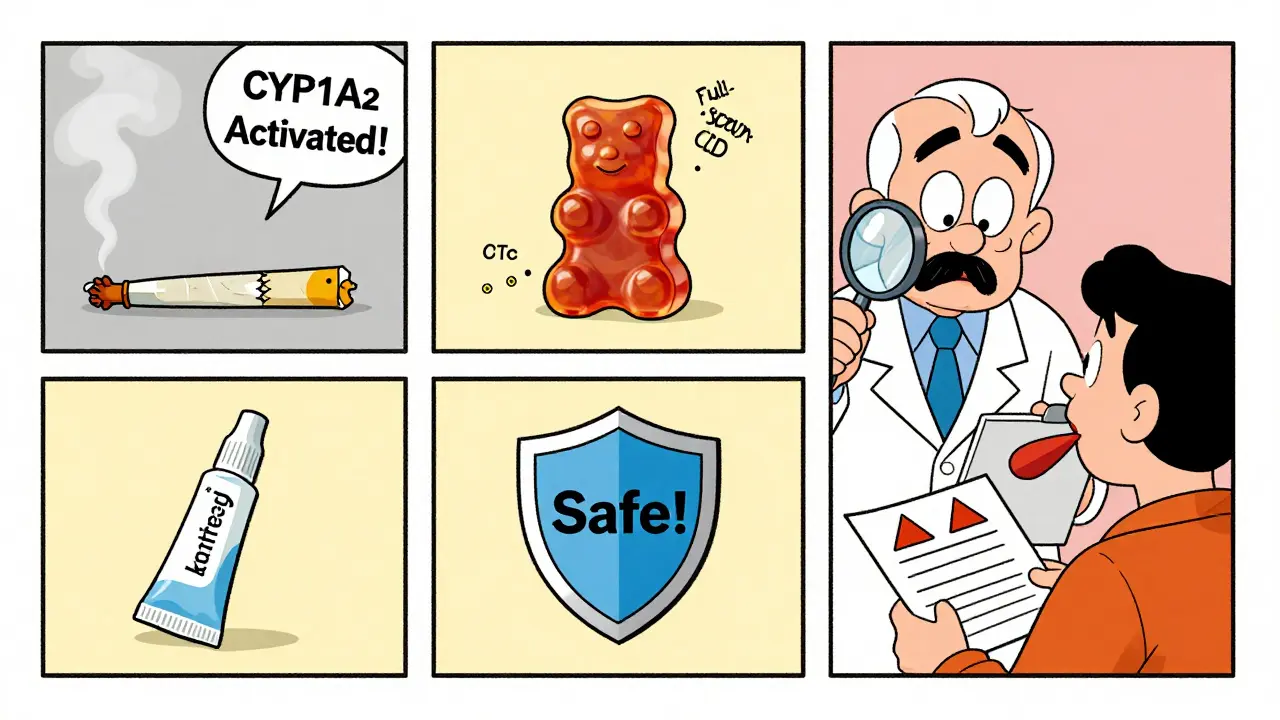
Cannabis doesn’t just sit there. It actively interferes with enzymes in your liver, especially the CYP450 family. These enzymes are responsible for breaking down about 60% of all prescription medications. Think of them as the body’s cleanup crew. When CBD or THC gets in the way, the cleanup slows down. That means your meds build up in your system.
CBD is a strong blocker of CYP3A4 and CYP2C19. THC hits CYP1A2, CYP2C9, and CYP3A4. These are the same enzymes that handle warfarin, clobazam, tacrolimus, and many others. When these enzymes are inhibited, drug levels can spike. A 2015 study found CBD increased clobazam levels by up to 500% in epilepsy patients. That’s not a small change - it’s enough to make someone too sedated to walk straight.
It’s not just oral CBD. Full-spectrum products - those with even trace amounts of THC - are 22-37% more likely to cause interactions than pure CBD isolates. That’s because THC and other cannabinoids work together in what’s called the "entourage effect." The more compounds in the product, the stronger the interference.
High-Risk Interactions: Don’t Take Chances
Some combinations are outright dangerous. The biggest red flags:
- Warfarin (Coumadin): CBD and THC inhibit CYP2C9, the enzyme that breaks down warfarin. In one review of 17 cases, INR levels jumped by 29-48% within 72 hours of starting CBD. That means your blood takes much longer to clot. One patient reported unexplained bruising after just one week. The American College of Clinical Pharmacy documented 12 cases of life-threatening bleeding linked to cannabis and warfarin.
- Tacrolimus and Cyclosporine: These are critical for transplant patients. THC and CBD can cause tacrolimus levels to rise 300-500% in just two days. That’s not a typo. A single dose of CBD oil can push someone into toxic territory, risking kidney failure or rejection.
- Anti-seizure drugs (like clobazam): In epilepsy patients, CBD is often used to reduce seizures - but it makes clobazam much stronger. A 2023 survey by the Epilepsy Foundation found 63% of users felt unusually sleepy. Many needed their clobazam dose cut by 25-40% just to function.
These aren’t theoretical risks. Real people are ending up in hospitals. The American Society of Health-System Pharmacists now recommends INR checks every 3-5 days for patients on warfarin who use cannabis - not the usual weekly check.
Moderate Risks: Watch for Changes
These interactions won’t kill you overnight, but they can make life harder:
- Benzodiazepines (alprazolam, diazepam): Both cannabis and these drugs calm the nervous system. Together, they can double sedation. In older adults, this increases fall risk by 47%, according to the Pennsylvania Pharmacists Association. One Reddit user wrote, "I couldn’t get out of bed without help after adding CBD to my Xanax."
- Opioids (oxycodone, morphine): Cannabis can slow how fast your body clears opioids. That means more pain relief - but also more risk of breathing problems. Studies show morphine clearance drops by 20-30%.
- Calcium channel blockers (amlodipine): These are used for high blood pressure. CBD can raise amlodipine levels by 30-40%. That can lead to dizziness, fainting, or dangerously low blood pressure.
These effects don’t always show up right away. They can creep in over days or weeks. That’s why people often don’t connect the dots until something goes wrong.

Low-Risk or Unclear Interactions
Not every interaction is a crisis. Some are minor or poorly supported by evidence:
- SSRIs (sertraline, fluoxetine): CBD may raise sertraline levels by 10-15%, but studies show almost no real-world impact. In a survey of 872 users, 41% reported no change at all.
- Statins (atorvastatin): Levels can rise 20-25%, but there’s no documented case of rhabdomyolysis (muscle damage) from this combo.
- Theophylline: This asthma drug behaves oddly. Smoked cannabis lowers its levels by 25-30% because it activates CYP1A2 - the opposite of what CBD does. So if you smoke, your asthma meds might stop working as well.
The key takeaway? Just because an interaction is "low risk" doesn’t mean it’s zero risk. Everyone’s body reacts differently.
Route of Use Matters
How you take cannabis changes how it interacts with your meds:
- Inhalation (smoking or vaping): THC hits your bloodstream in 6-10 minutes. That means sudden, short-term effects - like extreme drowsiness if you’re also on a sleeping pill.
- Oral (oils, edibles): CBD peaks in 2-4 hours and lasts 6-8. This creates a long window for interactions. If you take CBD at night with warfarin, your INR might spike the next morning - when you least expect it.
- Topicals: These rarely cause interactions because they don’t enter the bloodstream in significant amounts.
That’s why a patient using CBD oil for arthritis might have no issues - but if they switch to vaping THC for sleep, they suddenly feel foggy and unsteady. The product didn’t change. The delivery method did.
What You Should Do
If you’re on any prescription medication and thinking about using cannabis, here’s what to do:
- Be honest with your doctor. Don’t say "I use weed." Say: "I take 25 mg of CBD oil every night for anxiety. It’s full-spectrum."
- Check your meds. Use tools like the University of Washington’s Cannabis Drug Interactions database. It’s updated quarterly and free to use.
- Get baseline tests. If you’re on warfarin, tacrolimus, or clobazam, get blood levels checked before starting cannabis.
- Monitor closely. After starting cannabis, check INR or drug levels within 48-72 hours. Watch for new dizziness, sleepiness, bruising, or confusion.
- Adjust doses slowly. If your doctor recommends reducing your medication, do it by 10-25% - not half.
Pharmacists are often the best resource. But here’s the problem: 76% of community pharmacists in the U.S. say they feel untrained to advise on cannabis interactions. Don’t assume they know. Bring your own info.
Real Stories, Real Risks
Reddit’s r/MedicalCannabis has over 1,200 posts from people sharing their experiences. Common themes:
- "I started CBD oil and woke up with bruises all over my legs. My INR was 7.2. I almost bled out." - u/EpilepsyWarrior, March 2023
- "I’ve been on oxycodone for 10 years. Added 50mg CBD daily. No side effects. Still working fine." - u/ChronicPainSufferer, September 2022
- "My grandma fell three times in a week after adding CBD to her Xanax. She’s 78. We stopped it. She’s fine now." - u/GrandmaCaregiver, November 2022
These aren’t outliers. They’re warnings. One person’s safe experience doesn’t mean it’s safe for you.
The Bigger Picture
Cannabis use is growing fast. In 2022, over 58 million Americans used it - and 42% of them were also taking prescription drugs. Yet only 12 states require pharmacists to counsel patients on interactions. The FDA has received over 1,300 reports of possible cannabis-drug problems since 2018. Experts believe that’s less than 10% of actual cases.
Research is catching up. The NIH is funding a $2.3 million study on CBD and warfarin. The FDA launched a new clinical trials network in 2023. By 2027, experts expect clear guidelines for 85% of high-risk combinations. But right now? You’re on your own.
And there’s a blind spot: newer drugs like semaglutide (Ozempic) and other GLP-1 agonists. There’s almost no data on how cannabis affects them - even though 28% of cannabis users have diabetes. We’re flying blind in some areas.
Bottom Line
Cannabis isn’t harmless. Especially when mixed with other drugs. The risks aren’t hype - they’re documented in clinical studies, hospital reports, and patient stories. If you’re taking blood thinners, transplant meds, seizure drugs, or CNS depressants, you need to treat cannabis like any other medication: with caution, monitoring, and professional guidance.
Don’t assume it’s "natural" so it’s safe. Don’t assume your doctor knows. Don’t assume your pharmacist will tell you. Ask. Document. Test. Adjust. Your life could depend on it.
Can I take CBD with my blood thinner like warfarin?
No - not without close medical supervision. CBD and THC can increase warfarin levels by 29-48% within 72 hours, raising your INR to dangerous levels. This can lead to uncontrolled bleeding, internal hemorrhage, or stroke. If you’re on warfarin and want to use CBD, get your INR checked before starting, again 48-72 hours after, and then every 3-5 days until stable. Your doctor may need to reduce your warfarin dose by 10-25%.
Does CBD make anxiety meds like Xanax stronger?
Yes. Both CBD and benzodiazepines like alprazolam (Xanax) slow down your central nervous system. Together, they can cause extreme drowsiness, confusion, slowed breathing, and a 47% higher risk of falls in older adults. If you’re using both, start with low doses of CBD and watch for dizziness or trouble walking. Many people need to lower their Xanax dose by 20-30% to stay safe.
Is it safe to use CBD with antidepressants like sertraline?
For most people, yes - but monitor closely. CBD may raise sertraline levels by 10-15%, but studies show this rarely causes noticeable side effects. In one survey of 872 users, 41% reported no change at all. Still, if you notice increased nausea, jitteriness, or sleep changes after starting CBD, talk to your doctor. It’s low risk, but not zero risk.
What’s the difference between full-spectrum CBD and CBD isolate?
Full-spectrum CBD contains other cannabinoids, including up to 0.3% THC, terpenes, and flavonoids. These compounds work together and increase the chance of drug interactions - by 22-37% compared to pure CBD isolate. If you’re on medications that interact with cannabis, isolate is safer. But if you’re using it for pain or seizures, full-spectrum might be more effective. Talk to your doctor about which type fits your risk level.
How long after taking CBD should I wait before taking my medication?
There’s no proven timing rule. Some sources suggest taking CBD and medications 2 hours apart, but studies haven’t confirmed this reduces risk. The real solution is monitoring: check blood levels (like INR or drug concentrations) after starting CBD, not just timing. If you’re on warfarin or tacrolimus, timing won’t save you - only lab tests and dose adjustments will.
Can smoking cannabis affect my asthma medication?
Yes - but in the opposite way you might expect. Smoking cannabis activates the CYP1A2 enzyme, which speeds up the breakdown of theophylline (an older asthma drug). This can reduce its effectiveness by 25-30%, making your asthma worse. If you smoke and take theophylline, your levels need checking. CBD oils or edibles won’t do this - only smoking or vaping.
Do I need to tell my pharmacist if I’m using cannabis?
Absolutely. Pharmacists can spot dangerous interactions before you take a pill. But only 12 states require them to counsel patients on cannabis. Don’t wait for them to ask. Bring your product label and tell them exactly what you’re using - type, dose, and frequency. Many pharmacists want to help but don’t know how. Your information gives them the tools.





