Antacid & Antibiotic Timing Calculator
How to Use This Tool
Select your antibiotic type and antacid to see the recommended timing. Always consult your pharmacist or doctor for personalized advice.
Many people reach for an OTC antacid when their stomach feels off-heartburn, bloating, or that burning sensation after eating. It’s quick, easy, and works fast. But if you’re also taking antibiotics, you might be accidentally making your treatment less effective. This isn’t just a myth. It’s a well-documented, clinically significant interaction that can lead to treatment failure, longer illness, and even antibiotic resistance.
Why Antacids Interfere with Antibiotics
Antacids like Tums, Maalox, Mylanta, and Rolaids work by neutralizing stomach acid. They contain metal ions-aluminum, magnesium, calcium, or sodium bicarbonate-that bind to acid and reduce discomfort. But those same metal ions also bind to certain antibiotics, forming insoluble complexes that your body can’t absorb.Think of it like this: the antibiotic is trying to get into your bloodstream to fight infection. But the antacid grabs it and locks it up in your gut, where it just passes through unused. Studies show this can slash antibiotic absorption by 40% to 90%, depending on the drug and the antacid.
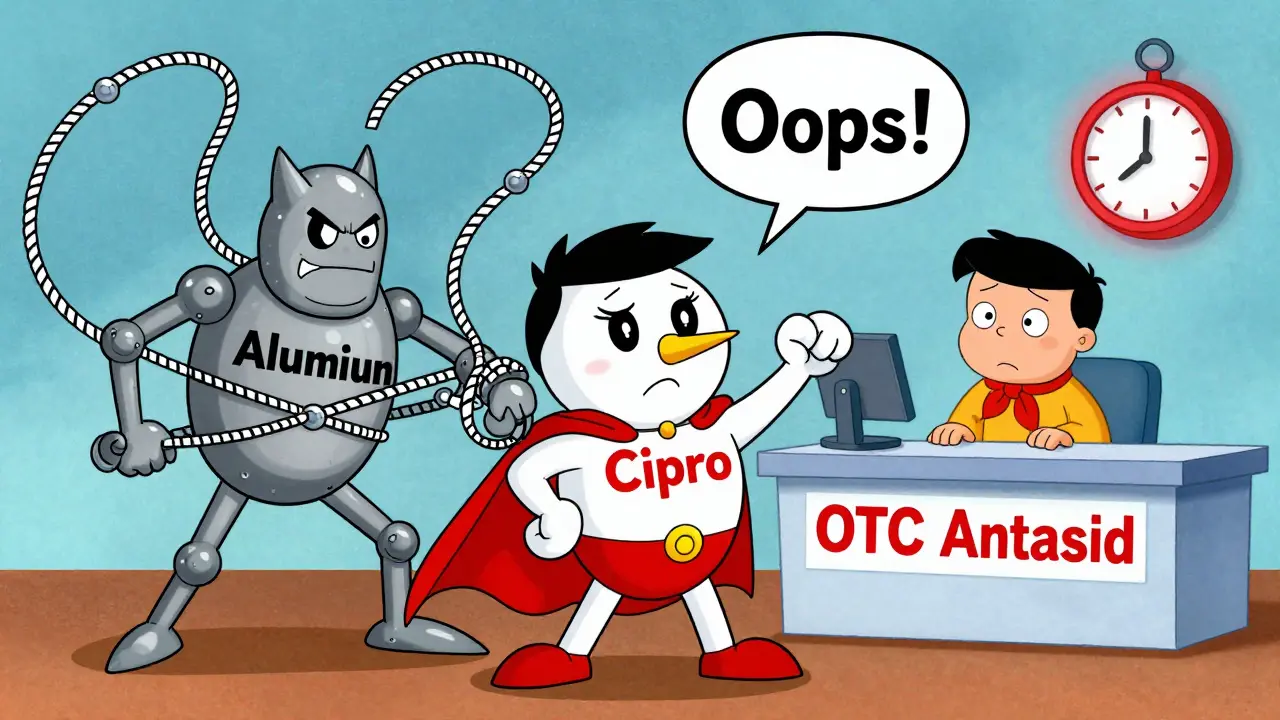
The biggest culprits are tetracyclines (like doxycycline and tetracycline itself) and fluoroquinolones (like ciprofloxacin and levofloxacin). For example, taking ciprofloxacin with an aluminum-containing antacid can drop its bioavailability from 70% to just 15-25%. That’s not a small drop-it’s the difference between a cure and a lingering infection.
Which Antibiotics Are Most Affected?
Not all antibiotics are equally vulnerable. Here’s what the data shows:- Tetracycline: Absorption drops 70-90% when taken with antacids containing aluminum or magnesium.
- Doxycycline: Still affected, though less severely-absorption reduced by 30-50%.
- Ciprofloxacin: One of the most impacted. A single antacid dose can cut absorption by 50-75%.
- Levofloxacin: Absorption reduced by 25-40%.
- Amoxicillin: Mixed results. Some studies show a modest 18-22% drop with aluminum-magnesium antacids; others show no significant effect, especially with amoxicillin-clavulanate.
- Penicillins, cephalosporins: Generally safe, but not risk-free. Always check with your pharmacist.
The key difference? Antibiotics that rely on being dissolved in an acidic environment or that have chemical structures prone to chelation (binding with metal ions) are the ones most at risk. Antacids don’t just change pH-they physically trap the drug molecules.
What About Other Acid Reducers?
If you need to manage stomach acid while on antibiotics, you might think H2 blockers (like famotidine) or proton pump inhibitors (PPIs like omeprazole) are safer. They are-mostly.Unlike antacids, these drugs don’t contain metal ions that chelate antibiotics. So they don’t form those insoluble complexes. But here’s the catch: they still raise stomach pH, which can affect how some antibiotics dissolve and absorb. For example, ketoconazole and itraconazole need acid to be absorbed, so PPIs can interfere with those antifungals. But for antibiotics like doxycycline or ciprofloxacin, PPIs and H2 blockers are generally much safer than antacids.
So if you’re on antibiotics and need acid relief, switching to famotidine or omeprazole for a few days might be a better choice. But don’t make that switch without talking to your doctor. These drugs aren’t harmless either-they have their own risks with long-term use.
How Long Should You Wait?
Timing matters more than you think. You can’t just take them together and hope for the best.Guidelines from the American Gastroenterological Association and the U.S. National Library of Medicine are clear:
- For tetracyclines and doxycycline: Take the antibiotic at least 2 hours before or 4-6 hours after the antacid.
- For fluoroquinolones like ciprofloxacin or levofloxacin: Wait 4-6 hours after taking the antacid before taking the antibiotic.
- For amoxicillin: While the risk is lower, it’s still wise to separate doses by at least 2 hours if you’re using aluminum- or magnesium-based antacids.
Why the difference? Fluoroquinolones bind more tightly to metal ions than tetracyclines do. That means they need more time to clear the gut before the antacid is even taken. If you take them too close together-even 30 minutes apart-you’re still risking reduced absorption.
And here’s something many people don’t realize: antacids don’t just work for an hour. Their effects can linger. So if you take one after dinner, and your antibiotic is due at bedtime, you’re still in the danger zone.
Real-World Consequences
This isn’t just theoretical. In clinical practice, this interaction causes real problems.A 2024 case study from University Hospitals described a patient with recurring urinary tract infections. She kept getting treated with ciprofloxacin, but the infections kept coming back. Her urine cultures never cleared. It wasn’t antibiotic resistance-it was timing. She was taking Tums (calcium carbonate) every day for heartburn. Once she stopped taking it within 4 hours of her antibiotic, her infection cleared on the next course.
A 2023 meta-analysis found that when antibiotics and antacids were taken too close together, treatment failure rates jumped by 37%. That means nearly 4 in 10 people weren’t getting better-not because the drug didn’t work, but because they never absorbed enough of it.
And then there’s the bigger picture: antibiotic resistance. When antibiotics don’t reach therapeutic levels, they don’t kill all the bacteria. The survivors multiply. Over time, that’s how resistant strains emerge. The CDC estimates over 35,000 deaths in the U.S. each year are linked to antibiotic-resistant infections. This interaction, though simple to fix, contributes to that crisis.
Who’s at Risk?
This isn’t just about older adults or people on lots of meds. It’s anyone who uses antacids regularly and gets prescribed an antibiotic.Here’s who needs to be especially careful:
- People with chronic heartburn or GERD who use antacids daily
- Elderly patients on multiple medications who don’t always read labels
- Parents giving antacids to kids for upset stomachs while also giving antibiotics
- Anyone who grabs an OTC antacid without thinking about their prescription
A 2022 survey found only 32% of OTC antacid users knew about the risk of antibiotic interactions-even though the warning is printed on the packaging. Most people assume if it’s sold over the counter, it’s harmless. That’s a dangerous assumption.

What Should You Do?
Here’s a simple, actionable plan:- Check your antibiotic. Is it a tetracycline or fluoroquinolone? If yes, treat it like a red flag.
- Check your antacid. Look at the active ingredients. Aluminum hydroxide? Magnesium hydroxide? Calcium carbonate? All risky.
- Separate doses. Take the antibiotic at least 2 hours before or 4-6 hours after the antacid. Use a timer if you have to.
- Ask your pharmacist. When you pick up your antibiotic, ask: “Does this interact with antacids?” They’re trained to catch this.
- Consider alternatives. If you need acid relief during your antibiotic course, ask your doctor about famotidine or omeprazole. They’re safer in this context.
Don’t stop taking your antibiotic because you’re worried. Don’t stop taking your antacid unless you have a better plan. Just space them out. That’s it.
What If You Already Took Them Together?
If you accidentally took your antibiotic and antacid at the same time, don’t panic. One mistake won’t ruin your treatment-but don’t make it a habit.Take your next dose on schedule, and make sure to separate them from now on. If you’re still feeling sick after a few days, or your symptoms are getting worse, contact your doctor. You might need a different antibiotic or a longer course.
And if you’re on antibiotics for a serious infection-like pneumonia, a kidney infection, or a severe skin infection-don’t gamble with timing. Be extra careful. Your health depends on it.
The Bottom Line
OTC antacids are convenient. Antibiotics are life-saving. But when they’re mixed up, the result can be ineffective treatment, longer illness, and even long-term public health risks.The fix is simple: know your drugs. Know your timing. Ask your pharmacist. And if you’re unsure, wait it out. A few extra hours between doses can mean the difference between getting better and having to start over.
This isn’t about avoiding antacids. It’s about using them wisely. Your body doesn’t care if something is sold over the counter. It only cares if it gets the right dose at the right time.
Can I take Tums with amoxicillin?
It’s generally safer than with tetracyclines or fluoroquinolones, but there’s still a small risk. Some studies show amoxicillin absorption can drop by 18-22% when taken with aluminum-magnesium antacids. To be safe, separate them by at least 2 hours. If you’re unsure, ask your pharmacist.
How long after taking an antacid can I take my antibiotic?
For tetracyclines like doxycycline, wait at least 2 hours after the antacid. For fluoroquinolones like ciprofloxacin, wait 4-6 hours. If you’re not sure which antibiotic you’re taking, aim for 4 hours-it covers most cases. Taking the antibiotic first, then waiting 2-4 hours before the antacid, is also acceptable.
Do all antacids interfere with antibiotics?
No. Antacids containing aluminum, magnesium, or calcium are the main problem because they bind to antibiotics. Sodium bicarbonate can also interfere, though less consistently. Antacids without these metals (like some newer formulations) may be safer, but they’re rare. Always check the active ingredients.
Can I take antacids at night if I take my antibiotic in the morning?
Yes, if you take your antibiotic in the morning and your antacid at night, you’re likely fine-assuming there’s at least 6-8 hours between doses. That’s usually enough time for the antibiotic to be absorbed before the antacid is introduced. But if your antibiotic is taken twice a day, make sure the timing still works for both doses.
Why don’t more people know about this?
Because it’s not obvious. Antacids are sold over the counter, and many people assume they’re harmless. The warnings are on the label, but they’re small and easy to miss. A 2022 survey found only 32% of users knew about the interaction. Pharmacists and doctors aren’t always reminded to mention it, either. Education gaps like this are why this interaction remains one of the top 3 most common OTC-prescription drug problems.