After giving birth, many new moms feel overwhelmed, tired, or emotional. That’s normal. But when those feelings don’t fade-when you can’t sleep even when the baby is sleeping, when you cry for no reason, or when you feel like you’re failing as a mother-that’s not just the baby blues. That’s postpartum depression. And it’s more common than you think. About 1 in 7 new mothers experience it. Left untreated, it can last for months or even years. But there’s help. One of the most studied and trusted options? Sertraline.
What is sertraline, really?
Sertraline is an antidepressant in a class called SSRIs-selective serotonin reuptake inhibitors. It works by helping your brain keep more serotonin, a chemical that affects mood, sleep, and appetite. Think of it like a gentle reset button for your brain chemistry. It’s not a quick fix. It doesn’t make you feel happy right away. But over time, it helps lift the fog so you can start feeling like yourself again.
It’s not new. Sertraline has been around since the 1990s. It’s sold under the brand name Zoloft, but generic versions are just as effective and much cheaper. It’s also one of the few antidepressants studied extensively in breastfeeding mothers. That’s important. Many women worry about taking medication while nursing. The good news? Sertraline passes into breast milk in very small amounts-so low that most pediatricians consider it safe for nursing babies.
Why sertraline over other options?
There are other SSRIs like fluoxetine (Prozac) or escitalopram (Lexapro). So why do doctors often pick sertraline for postpartum depression?
- Lower risk for babies: Studies show sertraline has the lowest transfer rate into breast milk among SSRIs. A 2023 review in Acta Psychiatrica Scandinavica found no significant side effects in infants exposed to sertraline through breastfeeding.
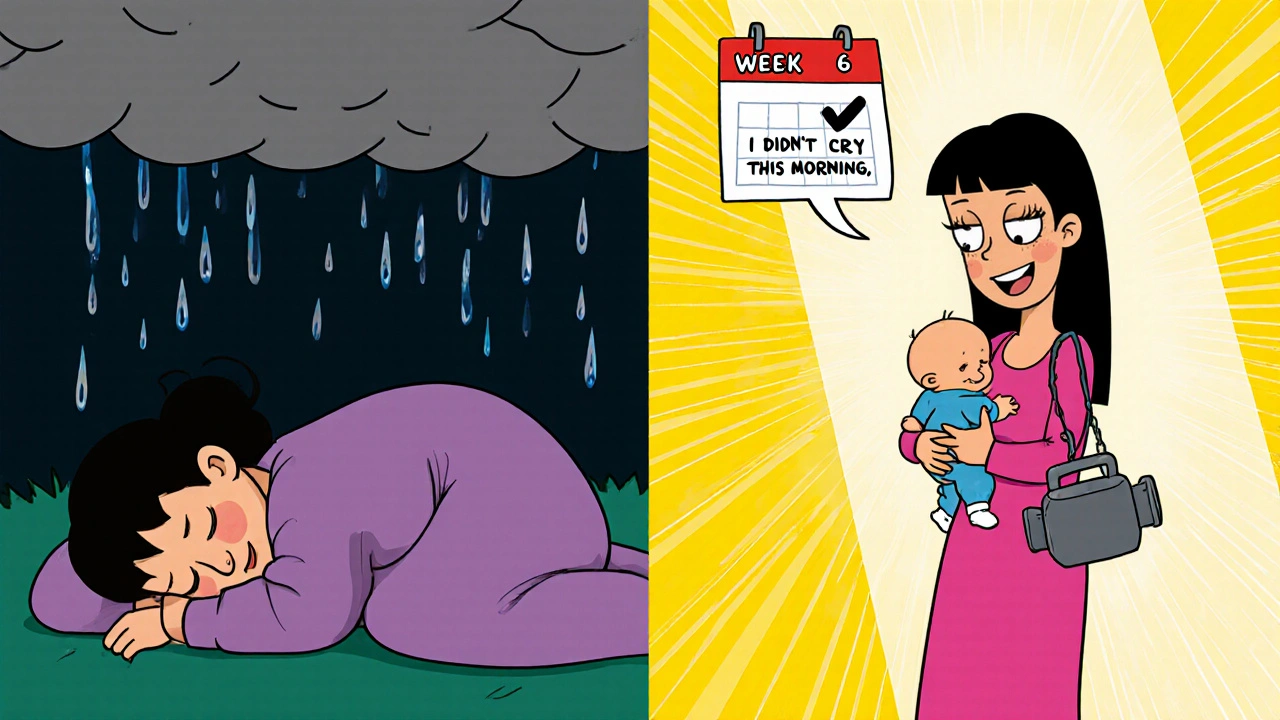
- Faster onset: Some women notice small improvements in mood within 2-3 weeks. Full benefits usually take 4-6 weeks.
- Lower chance of causing jitteriness: Unlike some other antidepressants, sertraline rarely causes restlessness or insomnia in new moms-two things you’re already battling with a newborn.
It’s not perfect. Some women report nausea, especially at first. Headaches or dry mouth can happen. But these usually fade after a week or two. If they don’t, your doctor can adjust the dose.
How does it work for postpartum depression?
Postpartum depression isn’t just sadness. It’s a mix of anxiety, guilt, exhaustion, and emotional numbness. Sertraline doesn’t erase your stress. It doesn’t fix your sleep schedule or make your partner do more laundry. But it helps your brain handle the stress better.
Think of it this way: after childbirth, your hormones drop faster than a rollercoaster. Your brain is trying to recalibrate. Sertraline helps smooth that ride. Many women say it’s like a weight lifting off their chest. They start noticing small joys again-the baby’s smile, a quiet cup of tea, a laugh with a friend.
One mom in Edinburgh, who asked to stay anonymous, shared: “I was crying every night. I felt like I was watching my life from outside. After three weeks on sertraline, I woke up and realized-I didn’t cry this morning. That was the first time in months.”
What about side effects?
Side effects are usually mild and short-lived. The most common ones:
- Nausea (take it with food)
- Headache
- Dry mouth
- Insomnia or drowsiness (can be managed by timing the dose)
- Reduced libido (this can happen with any SSRI)
Serious side effects are rare. But if you feel worse after starting sertraline-if you have sudden thoughts of self-harm or feel more anxious than before-call your doctor immediately. That’s unusual, but it can happen, especially in the first few weeks.
Also, don’t stop sertraline suddenly. If you want to quit, your doctor will help you taper off slowly. Stopping too fast can cause dizziness, brain zaps, or a return of depression symptoms.
Can you take it while breastfeeding?
Yes. And this is one of the biggest reasons sertraline is the go-to choice for new moms.
The American College of Obstetricians and Gynecologists (ACOG) and the Royal College of Psychiatrists in the UK both list sertraline as a preferred antidepressant during breastfeeding. Studies tracking babies exposed to sertraline through breast milk found no delays in development, no behavioral issues, and no increase in colic or feeding problems.
One 2024 study followed 120 breastfeeding mothers on sertraline. Their babies had normal weight gain, sleep patterns, and milestones at 6 and 12 months. That’s reassuring.
Still, if your baby seems unusually sleepy, fussy, or has trouble feeding, mention it to your pediatrician. It’s rare, but worth checking.
How long do you need to take it?
Most doctors recommend staying on sertraline for at least 6 to 12 months after symptoms improve. Stopping too soon increases the chance of depression coming back.
Some women stay on it longer-especially if they’ve had depression before, or if they’re still under a lot of stress. That’s okay. Antidepressants aren’t a life sentence. They’re a tool. You can stop when you’re ready, with your doctor’s help.
One thing to remember: you’re not weak for needing it. You’re not failing. You’re healing.
What else helps alongside sertraline?
Sertraline works best when paired with other support:
- Therapy: Cognitive behavioral therapy (CBT) helps you reframe negative thoughts. Many NHS services offer free postpartum CBT.
- Sleep: Even one extra hour of sleep a night can make a difference. Ask for help. Let someone hold the baby while you nap.
- Connection: Isolation makes depression worse. Join a local new moms’ group. Talk to someone who’s been there.
- Movement: A daily 20-minute walk outside boosts serotonin naturally. Sunshine helps too.
Medication alone won’t fix everything. But it can give you the energy and clarity to start doing the things that help.
When to talk to your doctor
You don’t need to wait until you’re at your lowest point. If you’ve felt down for more than two weeks after giving birth, if you’re avoiding your baby, if you feel like you’re not the person you used to be-it’s time to speak up.
Your GP or midwife can prescribe sertraline. You don’t need a specialist. If they hesitate, ask for a referral to a perinatal mental health team. They exist for this exact reason.
And if you’re scared about taking medication? That’s normal. But don’t let fear keep you stuck. You deserve to feel better. Sertraline has helped hundreds of thousands of new moms do exactly that.
Is sertraline safe for breastfeeding mothers?
Yes. Sertraline is one of the safest antidepressants for breastfeeding. It passes into breast milk in very low amounts, and multiple studies have found no harmful effects on infant development, feeding, or sleep. Major health organizations, including the UK’s Royal College of Psychiatrists and the American College of Obstetricians and Gynecologists, recommend it as a first-line option for nursing mothers.
How long does it take for sertraline to work for postpartum depression?
Some women notice small improvements in mood or energy within 2 to 3 weeks. But it usually takes 4 to 6 weeks for the full effect. Don’t give up if you don’t feel better right away. It’s not a quick fix-it’s a slow reset. If there’s no change after 6 weeks, talk to your doctor about adjusting the dose or trying another option.
Can sertraline cause weight gain?
Weight gain is possible, but it’s not common with sertraline compared to other antidepressants. Some people gain a few pounds due to improved appetite after depression lifts. Others don’t gain anything. If weight becomes a concern, talk to your doctor. Lifestyle changes like regular walking and balanced meals can help manage it.
Will sertraline make me feel numb or like a zombie?
No. That’s a myth. Sertraline doesn’t flatten your emotions. It helps lift the heaviness of depression so you can feel your feelings again-both the good and the bad. Many women say they start crying again, but this time it’s because they’re finally able to feel joy, relief, or even anger without being overwhelmed. It’s not about losing emotion-it’s about regaining balance.
Can I take sertraline if I’ve had depression before?
Yes. In fact, women with a history of depression are at higher risk for postpartum depression, and sertraline is often recommended as a preventive or treatment option. If you’ve responded well to sertraline in the past, your doctor may suggest starting it earlier-sometimes even right after birth-to prevent symptoms from returning.