When you’re taking anastrozole for breast cancer, your main focus is stopping the cancer from coming back. But what’s happening to your heart while you’re on it? Many patients don’t realize that lowering estrogen doesn’t just affect bones or hot flashes-it can change how your heart works. Anastrozole is a powerful drug, and its impact on cardiovascular health is real, measurable, and often overlooked.
How Anastrozole Works
Anastrozole is an aromatase inhibitor. It blocks the enzyme that turns androgens into estrogen. In postmenopausal women, most estrogen comes from fat tissue and other organs-not the ovaries-so anastrozole cuts estrogen levels by up to 80%. That’s why it’s so effective against hormone-receptor-positive breast cancer. But estrogen isn’t just a reproductive hormone. It plays a key role in keeping blood vessels flexible, helping cholesterol stay balanced, and reducing inflammation in the arteries.
When estrogen drops sharply, these protective effects fade. That’s not speculation. A 2021 analysis of over 12,000 postmenopausal women in the ATAC trial showed those taking anastrozole had a 17% higher risk of developing heart disease compared to those on tamoxifen. The difference wasn’t huge, but it was consistent across multiple studies. The risk doesn’t show up overnight. It builds over time, often after two or three years on the drug.
What Changes in Your Body
Lower estrogen affects several systems at once:
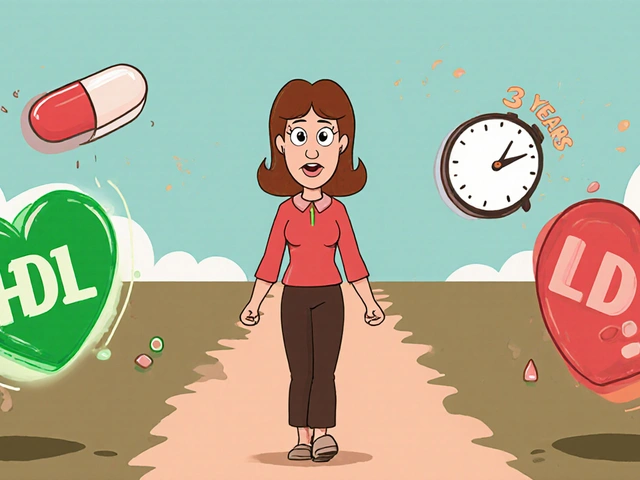
- Cholesterol levels: HDL (the good kind) tends to drop by 10-15%, while LDL (the bad kind) rises slightly. This shift increases plaque buildup in arteries.
- Blood pressure: Studies show a small but steady increase in systolic pressure-about 3-5 mmHg on average-over 5 years of treatment.
- Inflammation: Markers like C-reactive protein (CRP) rise in many women taking aromatase inhibitors, signaling low-grade vascular inflammation.
- Insulin resistance: Some women develop higher fasting glucose levels, increasing diabetes risk, which is itself a major heart disease factor.
These changes are subtle. You might not feel them. But they add up. Think of it like slow rust on a car’s frame-you don’t notice it until something breaks.
Who’s at Higher Risk?
Not every woman on anastrozole will have heart problems. But some are more vulnerable:
- Women over 65
- Those with pre-existing high blood pressure or high cholesterol
- People with a family history of heart disease
- Those who are overweight or sedentary
- Women who smoke or have had previous heart issues
If you’re in one of these groups, your doctor should be monitoring you more closely. A baseline lipid panel and blood pressure check before starting anastrozole is standard. But too often, follow-ups stop after the first year. That’s a gap. The biggest risks show up after 2-4 years of use.
What the Studies Say
Large clinical trials give us the clearest picture:
- ATAC Trial (2005-2015): 4,700 women on anastrozole had 1.6% more heart attacks and strokes over 10 years than those on tamoxifen.
- IBIS-II Trial (2017): Women on anastrozole had a 28% higher rate of cardiovascular events compared to placebo, even after adjusting for age and other factors.
- 2023 Meta-Analysis in JAMA Oncology: Reviewed 11 studies with 24,000+ patients. Found consistent 15-20% increased risk of major cardiovascular events with aromatase inhibitors, including anastrozole.
These aren’t rare side effects. They’re common enough that guidelines now recommend routine cardiovascular screening for women on long-term aromatase inhibitor therapy.
What You Can Do
You can’t stop anastrozole without risking cancer recurrence. But you can protect your heart while taking it.
- Get regular checkups: Ask for lipid panels every 6-12 months, not just once a year. Track your blood pressure at home if possible.
- Move daily: Just 30 minutes of brisk walking five days a week lowers heart disease risk by 30% in women on anastrozole, according to a 2022 study in the Journal of Clinical Oncology.
- Watch your diet: Focus on fiber, omega-3s (from fish or flaxseed), and avoid processed sugars. A Mediterranean-style diet has been shown to offset some of the negative lipid changes.
- Consider statins: If your LDL rises above 130 mg/dL, your doctor may recommend a low-dose statin. Studies show they’re safe and effective even with anastrozole.
- Don’t ignore symptoms: Unexplained fatigue, chest tightness, or swelling in the legs aren’t just "getting older." Get them checked.
Alternatives and Trade-Offs
If your heart health is a major concern, you might wonder: is there a better option?
| Drug | Heart Risk | Cancer Recurrence Risk | Common Side Effects |
|---|---|---|---|
| Anastrozole | Higher | Lower | Joint pain, bone loss, hot flashes |
| Letrozole | Similar to anastrozole | Similar | Same as anastrozole |
| Tamoxifen | Lower | Higher in postmenopausal women | Blood clots, uterine cancer risk |
| Exemestane | Similar to anastrozole | Similar | Androgenic effects (acne, hair growth) |
Tamoxifen has a better heart profile, but it’s less effective at preventing recurrence in postmenopausal women. It also carries its own risks, like blood clots and uterine changes. There’s no perfect choice-just different trade-offs. Your oncologist should help you weigh cancer risk against heart risk based on your personal history.
When to Talk to Your Doctor
Don’t wait for a crisis. Schedule a heart health checkup if:
- You’ve been on anastrozole for more than 2 years
- Your cholesterol or blood pressure has gone up
- You’re feeling more tired than usual
- You’ve gained weight around your waist
- You have a family history of early heart disease
Bring your latest lab results. Ask: "Is my heart at risk because of this drug? What can we do about it?" Most oncologists aren’t cardiologists, but they can refer you to one. A simple echocardiogram or coronary calcium scan can reveal hidden damage.
The Bottom Line
Anastrozole saves lives. But it doesn’t come without trade-offs. Ignoring heart health while taking it is like only checking the fuel gauge on a long road trip and forgetting to look at the tires. You might make it to your destination-but you could be in trouble before you get there.
The good news? Most of the heart risks are preventable. With regular monitoring, lifestyle changes, and smart medical decisions, you can take anastrozole and still protect your heart. You don’t have to choose between surviving cancer and staying healthy. You can do both.
Does anastrozole cause heart attacks?
Anastrozole doesn’t directly cause heart attacks, but it increases the risk over time by lowering estrogen, which normally protects blood vessels. Studies show a 15-20% higher chance of major cardiovascular events like heart attacks and strokes in women taking anastrozole compared to those on tamoxifen. The risk builds slowly, usually after 2-4 years of use.
Can I stop anastrozole if it’s affecting my heart?
Stopping anastrozole without medical guidance increases the risk of breast cancer returning. If you’re concerned about heart health, talk to your oncologist. They may adjust your treatment plan-like adding a statin, switching to tamoxifen (if appropriate), or extending therapy with closer monitoring. Never stop the drug on your own.
How often should I get my heart checked while on anastrozole?
At minimum, get a lipid panel and blood pressure check every 6-12 months. If you have risk factors like high cholesterol, diabetes, or obesity, your doctor may recommend more frequent checks. Home blood pressure monitoring and tracking weight or waist size can also help spot early warning signs.
Are there foods or supplements that help protect my heart on anastrozole?
Yes. Focus on a Mediterranean-style diet: olive oil, fatty fish like salmon, nuts, whole grains, and leafy greens. Omega-3 supplements (fish oil) may help lower triglycerides and reduce inflammation. Avoid sugary drinks and refined carbs, which worsen insulin resistance. Always check with your doctor before starting supplements-they can interact with other medications.
Is tamoxifen safer for the heart than anastrozole?
Yes, tamoxifen has a lower risk of heart disease than anastrozole. However, it’s less effective at preventing breast cancer recurrence in postmenopausal women and carries other risks, like blood clots and uterine cancer. The choice depends on your age, cancer stage, and personal health history. Your oncologist can help you decide which trade-off is right for you.
If you’re taking anastrozole, your body is fighting two battles at once: cancer and cardiovascular health. The good news is, you’re not powerless. Small, consistent actions-walking daily, eating well, getting tested-can make a big difference. You’re not just surviving treatment. You’re building a life after it.