Diacerein vs Alternatives Comparison Tool
Treatment Comparison Overview
Key Considerations
- Diacerein is the only proven DMOAD among oral agents for slowing cartilage loss
- NSAIDs offer rapid pain relief but carry CV and renal risks
- Glucosamine/Chondroitin are well-tolerated but show mixed evidence
- Hyaluronic Acid provides temporary joint lubrication
- Corticosteroids offer fast relief but risk cartilage damage with repeated use
Which Treatment Is Right for You?
Answer these questions to determine if Diacerein might be suitable:
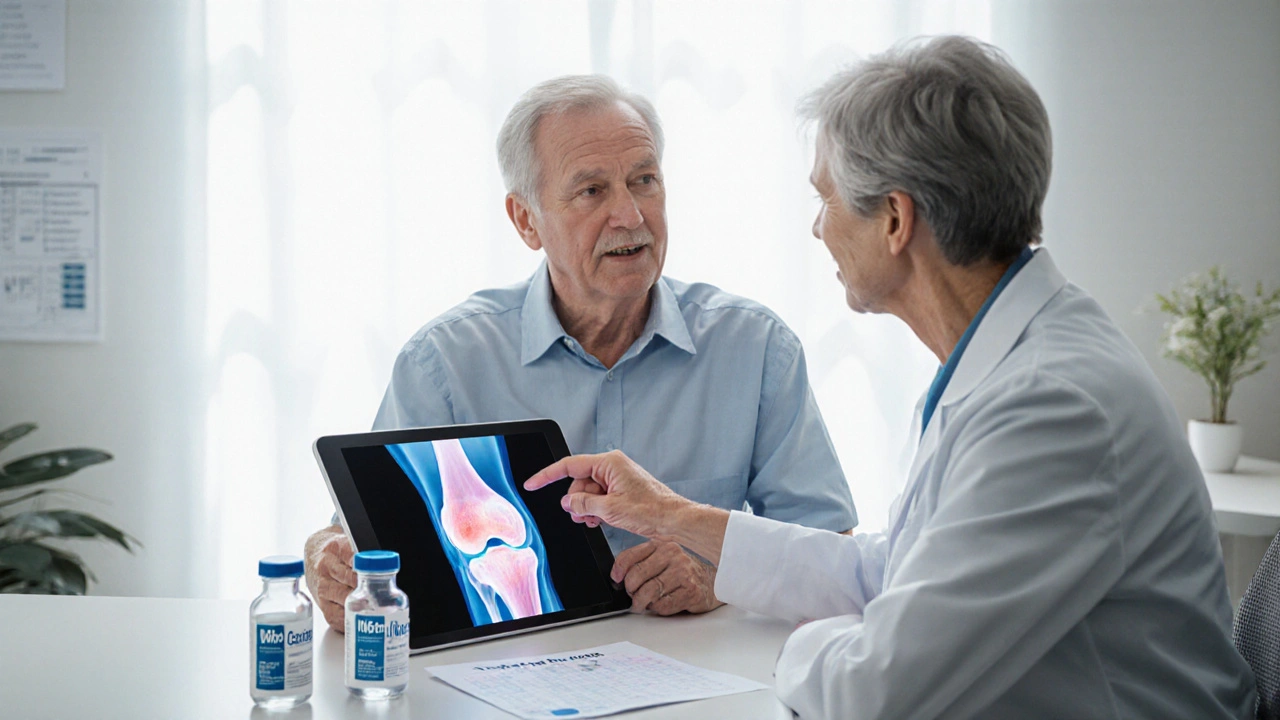
When it comes to managing osteoarthritis (OA), patients and clinicians often wonder whether a newer agent like Diacerein really offers an edge over the more familiar options. This guide breaks down how Diacerein works, weighs its benefits and risks, and puts it side‑by‑side with the common alternatives you’ll hear about in a typical OA clinic.
What is Diacerein?
Diacerein is a synthetic anthraquinone derivative marketed as a disease‑modifying osteoarthritis drug (DMOAD). It was first approved in Europe in the late 1990s for symptomatic OA of the knee and hip. The drug is taken orally, usually 50mg twice daily after meals.
How Diacerein Works
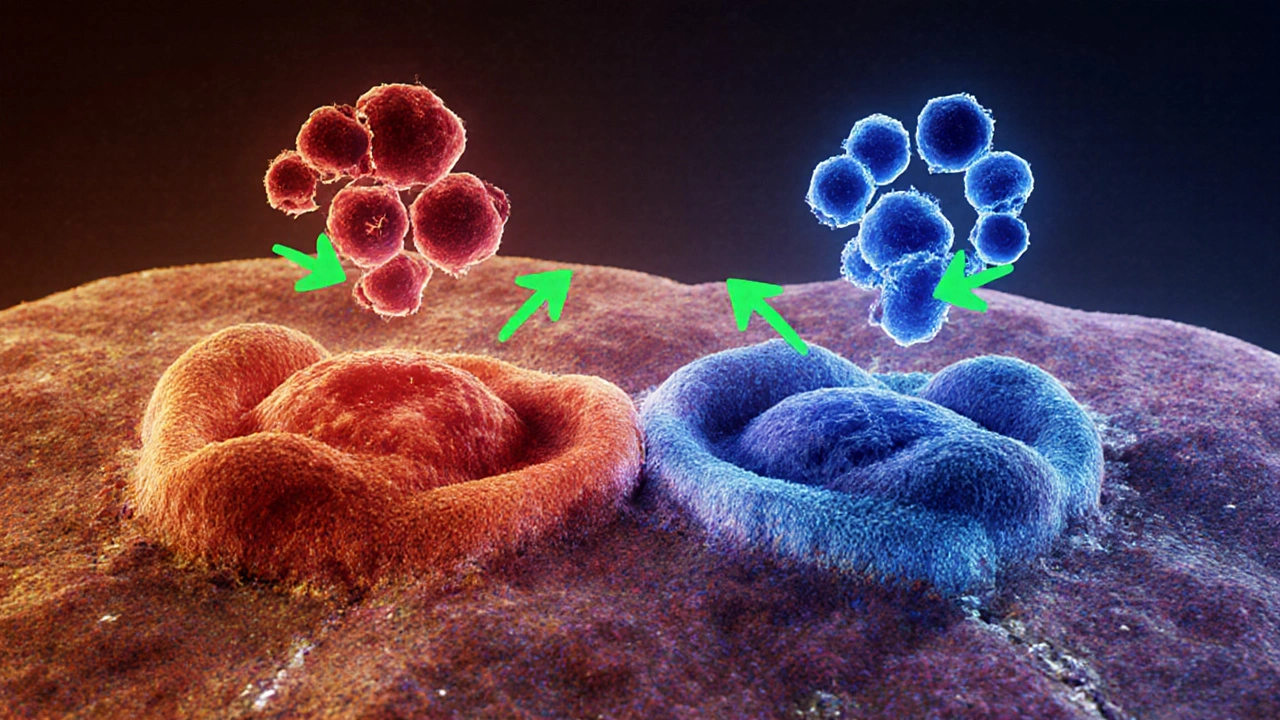
Diacerein’s key action is to curb the inflammatory cascade that drives cartilage breakdown. It inhibits the production of interleukin‑1β (IL‑1β) and reduces the activity of matrix metalloproteinases (MMPs), both of which chew away at the cartilage matrix. By dampening these enzymes, Diacerein aims to preserve cartilage thickness rather than just mask pain.
Clinical trials have shown a modest but statistically significant slowdown in joint space narrowing over 12‑month periods, suggesting a true structural benefit beyond symptomatic relief.
Safety Profile and Side Effects
Diacerein’s safety record is a mixed bag. The most common adverse events are gastrointestinal-especially loose stools and occasional abdominal cramps. These effects are dose‑related and tend to improve when the drug is taken with food. Rarely, liver enzyme elevations have been reported, so baseline liver function tests are advisable before starting therapy.
Because Diacerein does not inhibit cyclo‑oxygenase (COX) enzymes, it avoids the classic cardiovascular and renal risks associated with non‑steroidal anti‑inflammatory drugs (NSAIDs). This makes it an attractive option for older patients who have hypertension or a history of heart disease.
Common Alternatives to Diacerein
Below is a quick rundown of the most frequently prescribed OA agents, each introduced once with schema markup.
NSAIDs are oral or topical medications that relieve pain by blocking COX‑1 and COX‑2 enzymes, thereby reducing prostaglandin synthesis.
Glucosamine is a naturally occurring amino‑sugar that serves as a building block for glycosaminoglycans, the molecules that make up cartilage.
Chondroitin is a sulfated glycosaminoglycan often combined with glucosamine, thought to improve cartilage water retention and elasticity.
Hyaluronic Acid Injection delivers a high‑molecular‑weight gel into the joint space to lubricate and cushion the cartilage, providing temporary pain relief.
Corticosteroid Injection introduces a potent anti‑inflammatory steroid directly into the joint, often yielding rapid pain reduction.
Disease‑Modifying Osteoarthritis Drug (DMOAD) is a class label that includes agents, like Diacerein, that aim to alter the disease trajectory rather than merely alleviate symptoms.
Osteoarthritis is a degenerative joint disease characterized by cartilage loss, subchondral bone remodeling, and synovial inflammation.
Side‑by‑Side Comparison
| Attribute | Diacerein | NSAIDs | Glucosamine/Chondroitin | Hyaluronic Acid Injection | Corticosteroid Injection |
|---|---|---|---|---|---|
| Primary Action | IL‑1β inhibition, MMP reduction (DMOAD) | COX‑1/COX‑2 inhibition (analgesic) | Cartilage building block supplementation | Viscosupplementation, joint lubrication | Localized anti‑inflammatory effect |
| Onset of Pain Relief | 4-6 weeks (structural effect) | Within hours to days | Variable, often weeks | 1-2 weeks after injection | Within days |
| Effect on Cartilage | Slows joint‑space narrowing | No disease‑modifying effect | Mixed evidence, modest benefit | Temporary mechanical support | Potential cartilage loss with repeated use |
| Typical Side Effects | Loose stools, abdominal cramps, rare liver enzymes rise | Gastro‑intestinal ulceration, cardiovascular risk | Generally well tolerated, occasional GI upset | Injection site pain, transient swelling | Joint flare, possible cartilage damage |
| Contra‑indications | Severe hepatic disease, active GI disease | History of ulcer disease, renal insufficiency, heart failure | None specific | Active infection in joint | Uncontrolled diabetes, infection |
| Cost (per month) | ~£30‑£45 | ~£10‑£25 | ~£20‑£35 | ~£200‑£300 (single injection) | ~£150‑£250 (single injection) |
When to Choose Diacerein Over Other Options
Deciding whether Diacerein is the right fit hinges on three practical questions:
- Is the patient in need of disease‑modifying benefit? If the goal is to slow cartilage loss-especially in early‑to‑mid stage OA-Diacerein offers the only proven structural benefit among oral agents.
- Does the patient have cardiovascular or renal risk factors? Because Diacerein spares COX pathways, it’s safer than NSAIDs for patients with hypertension, chronic kidney disease, or a history of myocardial infarction.
- Can the patient tolerate mild gastrointestinal upset? If loose stools are a deal‑breaker, one might start at a low dose (50mg once daily) and titrate up, or opt for a different class altogether.
In practice, many clinicians reserve Diacerein for patients who have already tried NSAIDs with limited success or who cannot take NSAIDs due to comorbidities. It also fits well in a multimodal regimen that includes physiotherapy, weight management, and possibly a short course of NSAIDs for breakthrough pain.
Practical Tips for Prescribing Diacerein
- Start with 50mg once daily for the first week to gauge GI tolerance, then increase to the full 50mg twice daily.
- Advise patients to take the dose with meals; food helps reduce the stool‑related side effects.
- Order baseline liver function tests (ALT, AST) and repeat them after three months.
- Monitor bowel habits. If diarrhea persists beyond two weeks, consider dose reduction or a brief trial of a probiotic.
- Document the indication clearly-most insurers require proof of OA diagnosis and prior failure of NSAIDs.
Remember, Diacerein is not a rescue medication. It works best when patients maintain consistent use for at least three months before evaluating pain scores or functional improvement.
Frequently Asked Questions
Can Diacerein be taken together with NSAIDs?
Yes, short‑term co‑administration is common when breakthrough pain occurs. Because Diacerein does not increase gastrointestinal bleeding risk, combining it with a low‑dose NSAID for a few days is generally safe, but long‑term dual therapy should be avoided.
How long does it take to see a structural benefit from Diacerein?
Radiographic studies show a measurable reduction in joint‑space narrowing after 12‑18 months of continuous therapy. Patients should be counseled that pain relief may appear earlier, but cartilage protection is a long‑term goal.
Is Diacerein suitable for hand osteoarthritis?
Evidence is strongest for knee and hip OA. Small trials in hand OA suggest modest symptom relief, but clinicians often prefer topical NSAIDs or glucosamine‑chondroitin combos for this location.
What should I do if I develop liver enzyme elevation while on Diacerein?
Stop the medication immediately and repeat liver function tests within a week. If enzymes normalize, you may consider restarting at a lower dose under close monitoring. Persistent elevation warrants discontinuation.
Are there any herbal or natural products that work like Diacerein?
Some botanical extracts (e.g., Boswellia serrata) show anti‑IL‑1 activity, but none have robust clinical data comparable to Diacerein’s documented impact on cartilage metabolism.
Choosing the right OA therapy is rarely a one‑size‑fits‑all decision. By understanding how Diacerein stacks up against NSAIDs, supplements, and injectable options, you can tailor a plan that balances pain relief, safety, and long‑term joint health.