When you pick up a prescription, you might not think twice about whether the pill in your hand is the brand name or a cheaper generic. But behind that simple choice is a complex, science-backed system run by the FDA to make sure you get the same effect - safely and reliably. That system is called therapeutic equivalence codes, and it’s the reason pharmacists can swap out brand-name drugs for generics without asking your doctor every time.
What therapeutic equivalence really means
Therapeutic equivalence isn’t just about having the same active ingredient. It means two drugs - one brand, one generic - work the same way in your body. Same strength. Same form. Same route. And most importantly, they produce the same clinical result with the same safety profile. The FDA doesn’t guess at this. They require hard data.For a generic drug to be rated therapeutically equivalent, it must pass two major tests: pharmaceutical equivalence and bioequivalence. Pharmaceutical equivalence means the drugs have identical active ingredients, strength, dosage form, and route of administration. Bioequivalence means the generic drug enters your bloodstream at the same rate and to the same extent as the brand-name version. This isn’t just a theoretical standard. It’s measured through clinical studies, often using blood samples taken over time to track how quickly the drug is absorbed.
Without this level of proof, substitution could be risky. Imagine a generic version of a blood thinner that gets absorbed slower - that could lead to dangerous clots. Or one that hits too fast - risking bleeding. The FDA’s system exists to prevent exactly that.
The Orange Book and the code system
All this information is published in the FDA’s Approved Drug Products with Therapeutic Equivalence Evaluations, commonly known as the Orange Book. First released in 1980 and updated monthly, it’s the official source for therapeutic equivalence codes. Every multisource prescription drug - meaning any drug with more than one manufacturer - gets a code.The code is usually one or two letters. The first letter tells you everything you need to know:
- A means the drug is therapeutically equivalent to the brand-name version and can be substituted without hesitation.
- B means the FDA hasn’t found enough evidence to confirm equivalence. These drugs should not be substituted unless your doctor specifically approves it.
But it gets more detailed. After the A or B, there’s often a second letter - or even numbers - that give more context:
- AB is the most common code. It means the drug has passed bioequivalence studies and is fully substitutable.
- AB1, AB2, AB3, AB4 appear when multiple brand-name versions exist for the same drug. Each number points to a different reference drug. For example, if your prescription is for Brand A and you’re prescribed Generic X with code AB1, it means Generic X is equivalent only to Brand A - not Brand B.
- BC means extended-release products with potential bioequivalence issues. These are tricky because how the drug releases over time matters just as much as how much gets absorbed.
- BT is for topical products like creams or gels where skin absorption is hard to measure reliably.
- BN is for aerosol inhalers - where delivery to the lungs is complex and hard to replicate exactly.
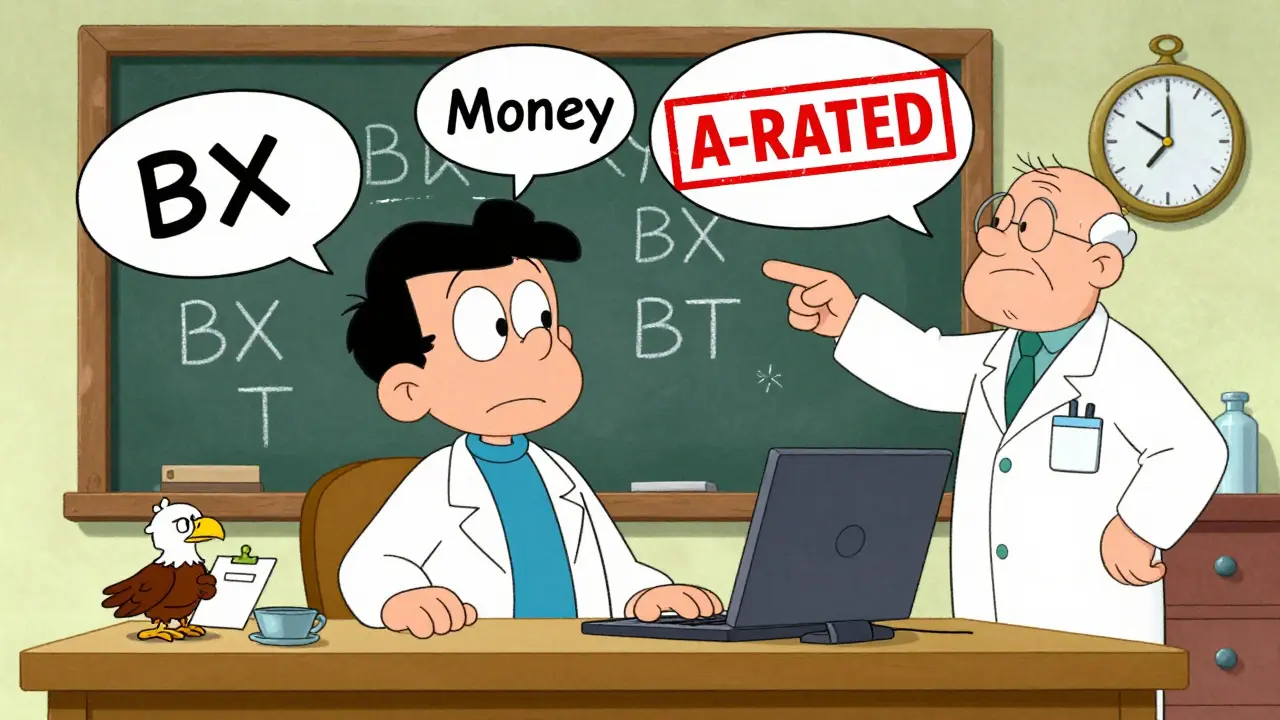
- BX means there’s not enough data to make a call. These are usually new or unusual products.
These codes aren’t just labels. They’re legal tools. In 49 states, pharmacists can legally substitute an A-rated generic without contacting your doctor. In most cases, they’re required to do so unless you or your doctor specifically says no.
Why some generics get B codes - and what it really means
Many people assume a B code means the generic doesn’t work. That’s not true. It means the FDA doesn’t have enough data to say it’s equivalent - not that it definitely isn’t.Take topical corticosteroids. A cream might have the same active ingredient and concentration as the brand, but if the base (the lotion or ointment part) is different, it can change how much gets into your skin. Standard blood tests can’t measure that. So the FDA gives it a BT code - not because it’s unsafe, but because they can’t prove it works the same way.
Same with complex injectables or inhaled drugs. These aren’t simple pills. Their effectiveness depends on particle size, delivery mechanism, and how the body absorbs them. Traditional bioequivalence studies just don’t capture all that. So even if the generic is made by the same company as the brand, it might still get a B code.
And here’s the problem: doctors often don’t know what B codes mean. A 2022 American Medical Association survey found that 42% of physicians were confused by them. Some think a B-rated drug is inferior. Others don’t realize they can still prescribe it - they just can’t automatically substitute it. This leads to confusion at the pharmacy and sometimes, unnecessary costs.
How pharmacists use the system
Pharmacists are the frontline users of the Orange Book. Every time a prescription comes in for a brand-name drug, they check the TE code before dispensing. Most use pharmacy software that auto-populates the code, but many still pull up the FDA’s website directly - especially for complex cases.According to a 2022 survey by the National Community Pharmacists Association, 87% of pharmacists say TE codes make substitution faster and safer. They spend about 2.7 minutes per prescription verifying the code. That might sound like a lot, but it saves time in the long run. Instead of calling doctors to confirm substitutions, they can act with confidence.
But it’s not foolproof. In 28% of cases, pharmacists have refused to substitute a B-rated drug that was actually appropriate - not because the code said no, but because they didn’t understand the context. A drug with a BC code for extended-release might still be safe to swap if the prescriber knows the patient has been stable on it. But without clear communication, pharmacists play it safe - and patients pay the price.
Why the system works - and where it’s falling short
The U.S. therapeutic equivalence system is the most advanced in the world. The European Medicines Agency doesn’t use codes at all - they publish detailed scientific reviews. That’s useful for experts, but not practical for a pharmacist filling 50 prescriptions an hour.Here in the U.S., over 90% of generic drugs carry an A rating. That’s why generics make up 90% of prescriptions but only 23% of drug spending - saving the system about $370 billion a year.
But the system was built for simple pills. It’s struggling with today’s complex drugs. Between 2018 and 2022, the number of B-rated applications for complex generics like inhalers, topical products, and injectables rose by 22%. These aren’t easy to test. Standard blood tests don’t show how well a cream penetrates skin or how evenly an inhaler delivers medicine to the lungs.
The FDA knows this. In 2022, they released a draft guidance proposing new ways to evaluate these products - using better lab methods, real-world data, and even patient outcomes. Their goal? Cut B-rated products for complex generics by 30% by 2027.
What this means for you
If you’re on a generic drug and your pharmacist switches it, you’re probably fine. The system works - and it’s saved billions.But if you’re on a complex drug - like an inhaler, a topical cream, or an injectable - and you notice a change in how you feel after switching to a generic, speak up. It might not be the drug’s fault, but it might be worth checking with your doctor.
And if your doctor prescribes a brand-name drug without specifying "dispense as written," ask if there’s an A-rated generic. You could save money without risking your health.
The FDA’s therapeutic equivalence codes aren’t perfect. But they’re the best tool we have to make sure generic drugs are safe, effective, and affordable. And for most people, that’s exactly what they need.
What does an AB code mean on a generic drug?
An AB code means the generic drug has been proven to be therapeutically equivalent to the brand-name version. It has the same active ingredient, strength, dosage form, and route of administration, and has passed bioequivalence testing. Pharmacists can substitute it without needing approval from your doctor.
Can I always substitute an A-rated generic for a brand-name drug?
In 49 U.S. states, yes - pharmacists are allowed to substitute A-rated generics without contacting your doctor. However, some states require them to notify you or your prescriber. Always check your state’s pharmacy laws. Also, if your doctor writes "dispense as written" or "no substitution," the pharmacy must follow that instruction.
Why do some generic drugs have a B code?
A B code means the FDA doesn’t have enough data to confirm the generic is therapeutically equivalent to the brand. This often happens with complex products like inhalers, topical creams, or extended-release tablets, where traditional blood tests can’t fully measure how the drug works in the body. A B code doesn’t mean the drug is unsafe - just that substitution isn’t automatically approved.
Are over-the-counter (OTC) drugs given therapeutic equivalence codes?
No. The FDA’s therapeutic equivalence system only applies to prescription drugs. OTC medications are regulated under different standards and are not listed in the Orange Book or assigned TE codes.
How often is the Orange Book updated?
The Orange Book is updated monthly by the FDA to reflect new drug approvals, code changes, and withdrawals. You can access the latest version for free on the FDA’s website. Pharmacists and prescribers rely on these updates to make accurate substitution decisions.