Switching from brand-name Coumadin to a generic version of warfarin sounds simple-cheaper, same drug, right? But for patients on warfarin, that switch isn’t just a pharmacy change. It’s a medical event that can ripple through their entire treatment plan. Warfarin isn’t like most pills. It’s a warfarin with a razor-thin safety margin. Too little, and you risk a stroke or blood clot. Too much, and you could bleed internally without warning. That’s why INR monitoring isn’t optional-it’s life-saving. And when you switch generic brands, even if the FDA says they’re "therapeutically equivalent," your body might react differently.
Why Warfarin Is Different
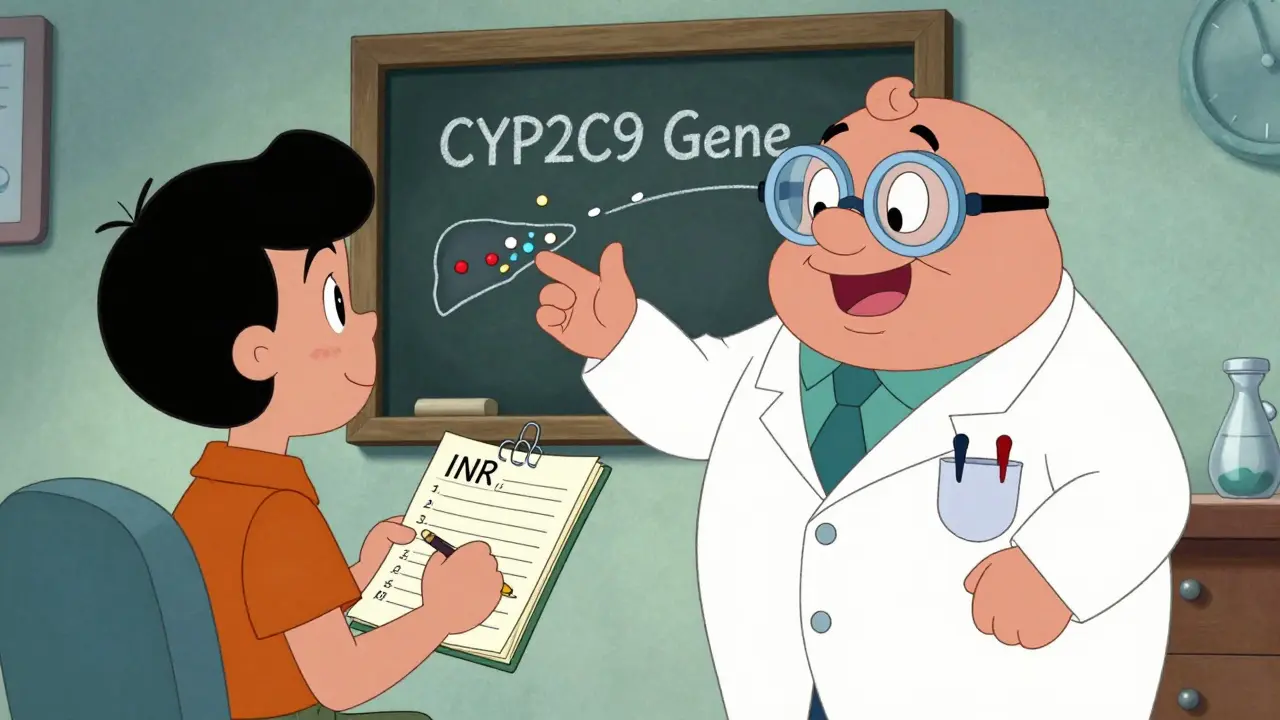
Warfarin has been around since the 1950s, and it’s still used by over 1.2 million Americans today. It works by blocking vitamin K, which your body needs to make clotting factors. But the difference between a safe dose and a dangerous one is tiny. The target INR range for most people is 2.0 to 3.0. For someone with a mechanical heart valve, it’s even tighter: 2.5 to 3.5. Go outside that range, even by 0.5, and your risk of bleeding or clotting jumps sharply.What makes warfarin tricky isn’t just the dose-it’s how your body handles it. It’s broken down by liver enzymes (CYP2C9 and CYP3A4), and those enzymes can be affected by dozens of other drugs, foods, and even changes in your gut bacteria. A new antibiotic, a sudden increase in leafy greens, or skipping a dose can throw your INR off in just a few days. That’s why frequent testing is non-negotiable, especially when you’re first starting or switching formulations.
Generic Warfarin Isn’t All the Same
There are currently 12 FDA-approved generic warfarin sodium products from eight different manufacturers. They all meet the same bioequivalence standards: their absorption (AUC) and peak concentration (Cmax) must fall within 80-125% of Coumadin. Sounds good, right? But here’s the catch: those standards were designed for drugs with wide therapeutic windows-like antibiotics or blood pressure pills. Warfarin isn’t one of them.Studies show that for most patients, switching from Coumadin to a single generic brand-like the Barr Laboratories version studied in the 2002 Witt trial-doesn’t cause major problems. INR levels stayed stable, and bleeding or clotting events didn’t increase. But when patients switch between different generic brands-say, from Teva to Mylan to Sandoz-that’s when things get risky. One patient might handle the switch fine. Another might see their INR spike from 2.8 to 4.5 in a week, with no obvious reason. That’s not rare. Around 15-20% of patients need closer monitoring after switching between generic manufacturers.
The FDA says all approved generics are equivalent. But they also admit: "Individual patient responses may vary." That’s not a disclaimer-it’s a clinical reality.
When You Switch, Monitor Like You’re Starting Over
If you’re switching from Coumadin to a generic, or from one generic to another, treat it like you’re just beginning warfarin therapy. Don’t assume stability. Don’t wait for your next scheduled check. Here’s what the experts recommend:- Check your INR within 3 to 5 days after the switch.
- Check again in 3 to 7 days.
- Continue checking every 3 to 7 days for the next 2 weeks, or until your INR has been stable for two consecutive tests.
- Only then should you return to your usual monitoring schedule (every 4-6 weeks if stable).
Some clinics, like the Cleveland Clinic, even recommend daily or every-other-day INR checks for the first week after switching. That might sound intense, but consider this: in one 2017 study, nearly half of patients who had unexplained INR changes after switching generics had no other identifiable cause-no new meds, no diet changes, no missed doses. The switch itself was the trigger.

What to Watch For After the Switch
Even with careful monitoring, something might still go wrong. If your INR suddenly jumps or drops without explanation, ask these questions:- Did you switch pharmacies or generic brands recently?
- Have you eaten more or less vitamin K? Spinach, kale, broccoli, and Brussels sprouts can all affect warfarin. A 100-150 mcg daily change in vitamin K intake can shift your INR.
- Have you started or stopped any other medications? Antibiotics, antifungals, aspirin, NSAIDs, even some herbal supplements like garlic or ginkgo can interact.
- Did you miss a dose? Non-adherence affects 15-30% of warfarin users.
- Was the blood test done at the same lab? Different labs can have slightly different INR calibration.
If none of these explain the change, your doctor should consider the generic switch as the likely culprit. A small dose adjustment-usually 5-10% up or down-often fixes it. But don’t adjust it yourself. Warfarin isn’t a trial-and-error drug.
Warfarin vs. DOACs: The Real Trade-Offs
You’ve probably heard about the newer anticoagulants-apixaban, rivaroxaban, dabigatran. They don’t need INR checks. They have fewer food interactions. They’re easier. But they cost 30 to 50 times more than generic warfarin. A month of warfarin runs $4-$10 with insurance. A month of a DOAC? $300-$500.For many people-especially those on Medicare, Medicaid, or without good drug coverage-warfarin is the only realistic option. It’s also the only choice for people with mechanical heart valves, severe kidney disease, or antiphospholipid syndrome. DOACs don’t work well for those groups.
And here’s something else: if you bleed badly on warfarin, doctors can reverse it fast-vitamin K, fresh frozen plasma, or a specific antidote (idarucizumab for dabigatran, but not for warfarin). With DOACs, reversal is harder, slower, or sometimes impossible.
So it’s not just about cost. It’s about control, access, and emergency readiness.
What You Can Do to Stay Safe
If you’re on warfarin, here’s how to protect yourself:- Always know which generic brand you’re taking. Write down the manufacturer name (Teva, Mylan, Sandoz) and pill color/shape. If your pharmacy switches it without telling you, ask why.
- Keep a log of your INR results, doses, and any symptoms (bruising, nosebleeds, dark stools, headaches).
- Don’t change your diet suddenly. Eat consistent amounts of vitamin K-rich foods.
- Tell every doctor, dentist, and pharmacist you’re on warfarin-even for a simple antibiotic.
- If you’re switched to a new generic, insist on INR checks every 3-7 days for the first two weeks.
- Ask your doctor about genetic testing for CYP2C9 and VKORC1. Some people metabolize warfarin much slower or faster based on their genes. That info can help predict how you’ll respond to a switch.
The Bottom Line
Generic warfarin is safe-for most people, most of the time. But "safe" doesn’t mean "no risk." The data shows that switching between different generic manufacturers can cause INR instability in a significant number of patients. That’s not a failure of the generics. It’s a failure of one-size-fits-all thinking.Warfarin demands attention. It’s not a pill you take and forget. It’s a treatment that requires partnership-with your doctor, your pharmacist, and yourself. If you’re switching generics, don’t assume everything will be fine. Push for monitoring. Track your numbers. Speak up if something feels off. Because when it comes to warfarin, the difference between safety and danger is often just a fraction of an INR point.
Can I switch between different generic warfarin brands without checking my INR?
No. Switching between different generic manufacturers-even if they’re both FDA-approved-can cause your INR to rise or drop unexpectedly. Always check your INR within 3-5 days after switching, and continue frequent testing for at least two weeks until your levels stabilize.
Is generic warfarin as effective as Coumadin?
For most patients, yes. Large studies show that switching from Coumadin to a single generic brand doesn’t increase bleeding or clotting risks. But if you switch between multiple generic brands over time, your body may respond differently to each formulation. Consistency in the manufacturer helps maintain stable INR levels.
Why does my INR keep changing even though I haven’t changed my dose or diet?
If your INR fluctuates without clear reasons like diet, medications, or missed doses, the generic brand you’re taking could be the cause. Different manufacturers use slightly different inactive ingredients or manufacturing processes, which can affect how your body absorbs the drug. This is especially common with warfarin because of its narrow therapeutic index.
Should I ask my doctor to prescribe only one brand of generic warfarin?
Yes, if possible. Ask your doctor to write "Dispense as written" or "Do not substitute" on your prescription if you’ve found a generic brand that works well for you. This helps prevent your pharmacy from switching you to another manufacturer without your knowledge.
Are there alternatives to warfarin that don’t need INR monitoring?
Yes-direct oral anticoagulants (DOACs) like apixaban and rivaroxaban don’t require regular INR tests. But they’re much more expensive and aren’t suitable for everyone, especially people with mechanical heart valves or severe kidney disease. Warfarin remains the best option for many patients due to its low cost and proven reversibility in emergencies.