When opioids work, they work well. For someone with severe pain after surgery or cancer, these drugs can mean the difference between suffering and relief. But for many, what starts as medical necessity turns into a dangerous cycle: needing more to feel the same effect, then becoming physically dependent, and in the worst cases, dying from an overdose. It’s not a story of weak willpower. It’s a story of biology - and how the body adapts in ways that can be deadly.
How Opioids Change Your Brain
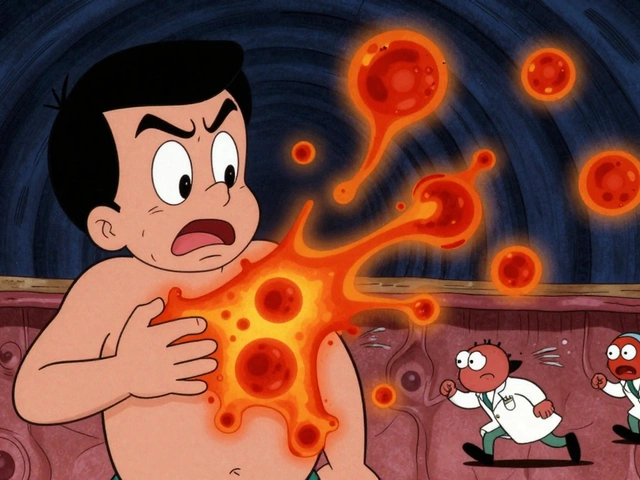
Opioids bind to special receptors in your brain, spinal cord, and gut. These receptors are meant to respond to your body’s own painkillers - chemicals like endorphins. But opioids are stronger. They flood the system, triggering a rush of dopamine that brings relief - and sometimes euphoria. That’s why they’re effective. But that same mechanism is what makes them risky.
With repeated use, your brain starts to adjust. The receptors become less sensitive. This is called tolerance. You need higher doses to get the same pain relief. Or, if you’re using recreationally, the same high. It’s not a choice. It’s a chemical shift. Studies show that within six months of chronic opioid use, most patients need 25% to 50% more medication just to manage the same level of pain.
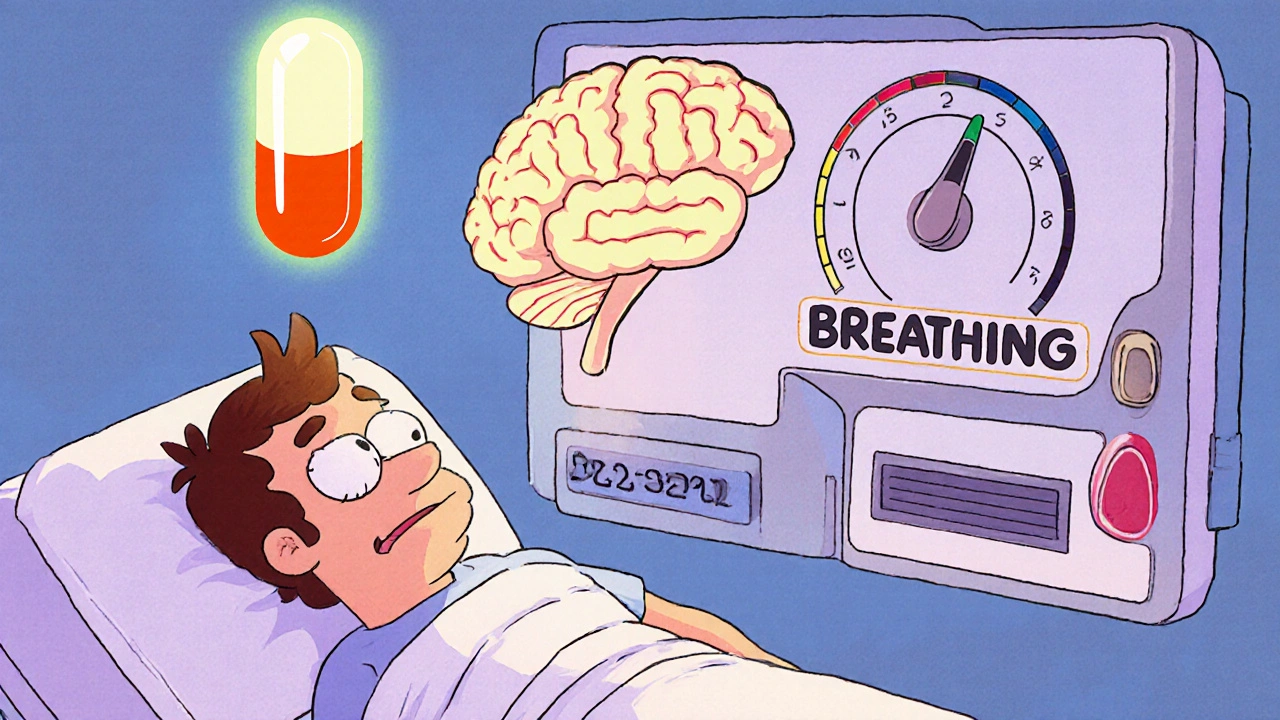
And here’s the trap: tolerance to pain relief and euphoria develops faster than tolerance to respiratory depression - the dangerous slowing of breathing that can kill you. That’s why someone who’s been using opioids for years can still overdose. Their body has learned to handle the high, but not the shutdown of breathing.
Dependence Isn’t Addiction - But It’s Still Dangerous
Tolerance often leads to physical dependence. That means your body now relies on the drug to function normally. If you stop suddenly, you get sick. Symptoms include nausea, vomiting, muscle aches, anxiety, and insomnia. This isn’t weakness. It’s your nervous system screaming for the chemical it’s come to expect.
Dependence doesn’t always mean addiction. Someone on a low, stable dose of oxycodone for chronic back pain might be dependent but not using it compulsively or chasing highs. But for others, dependence becomes addiction - a compulsive need to use despite harm. The line is blurry. What matters is the risk: dependence makes quitting harder. And quitting without support can be deadly.

Overdose: Why It Happens - Even to Experienced Users
Overdose isn’t just about taking too much at once. It’s about the mismatch between your body’s current tolerance and the dose you take.
Take fentanyl. It’s 50 to 100 times stronger than morphine. A tiny amount - as little as 2 milligrams - can stop breathing. Illicit fentanyl is now mixed into heroin, counterfeit pills, and even cocaine. People think they’re taking oxycodone. They’re not. They’re getting a lethal dose.
Even long-term users aren’t safe. Research from the National Institute on Drug Abuse shows that tolerance to respiratory depression never fully develops. That means your breathing control system never fully adapts. A small increase in dose - or mixing opioids with alcohol, benzodiazepines, or sleep aids - can push you over the edge.
And then there’s relapse. People who’ve been clean for weeks or months lose their tolerance. But their cravings don’t vanish. They take their old dose - the one that used to work. And it kills them. Data from the Journal of Substance Abuse Treatment shows 65% of opioid overdose deaths happen in people who’ve had prior treatment. One Reddit user wrote: “After 6 months clean, I used my old dose and nearly died - paramedics said I was clinically dead for 4 minutes.” That’s not rare. It’s predictable.
Not All Opioids Are the Same
Some opioids carry higher risks than others. Fentanyl and heroin are the biggest killers. Methadone, while used for treatment, has a long half-life and can build up in the body, increasing overdose risk if dosed incorrectly.
Buprenorphine is different. It’s a partial agonist. That means it activates opioid receptors - enough to reduce cravings and withdrawal - but not enough to cause severe respiratory depression. It has a ceiling effect: after a certain dose, it doesn’t get stronger. That’s why it’s safer. It’s why it’s used in Medication-Assisted Treatment (MAT). And it’s why the 2023 MAT Act removed the old licensing requirement (the X-waiver), allowing any licensed doctor to prescribe it. That change alone could save thousands.
Even morphine and oxycodone have risks - but they’re better understood. When used properly under medical supervision, they can be managed. But when taken without oversight, or mixed with other depressants, they become a gamble with your life.
What’s Being Done - And What Still Needs to Change
Prescription rates have dropped since their peak in 2012. In 2021, doctors wrote less than half the number of opioid prescriptions they did a decade earlier. That’s progress. But the gap has been filled by illicit fentanyl. Between 2015 and 2022, fentanyl seizures in the U.S. increased by 1,200%.
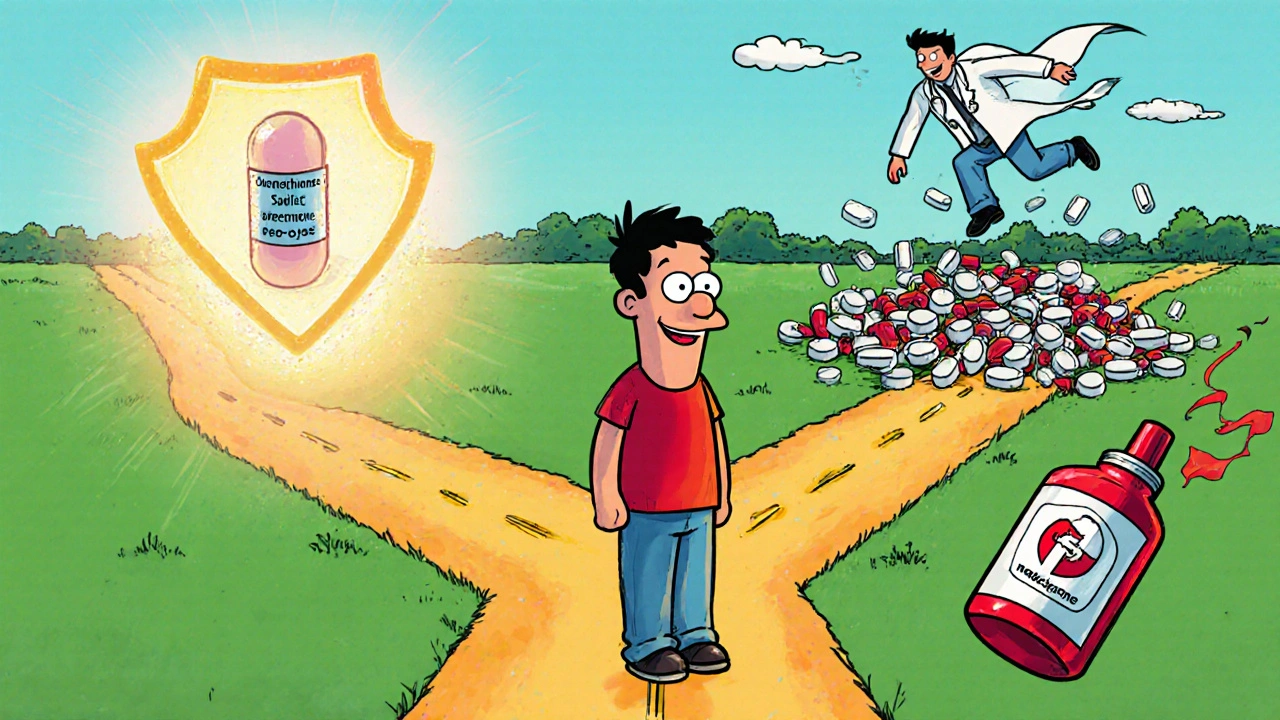
Efforts to reduce harm are growing. Naloxone - the overdose reversal drug - is now available without a prescription in most states. Communities that distribute it widely have seen fatal overdoses drop by 34%. Harm reduction groups report that 87% of the overdoses they reverse involve people who had previously been in recovery. That’s the lost-tolerance effect in real time.
Research is pushing forward too. New drug formulations like AVERSION technology try to make pills harder to crush or inject. Scientists are exploring “biased ligands” - opioids that relieve pain without triggering respiratory depression. If they work, they could change everything.
But the biggest tool we have right now is access to treatment. MAT with buprenorphine or methadone cuts overdose risk by half. Yet only a fraction of people who need it get it. Stigma, cost, and lack of providers still block access. And until that changes, the cycle will keep turning.
What You Need to Know - Whether You’re a Patient, a Loved One, or Just Curious
- If you’re prescribed opioids, ask: Is this the lowest effective dose? How long will I need it? Are there non-opioid options?
- Never mix opioids with alcohol, sleeping pills, or anxiety meds. That combo is a leading cause of overdose.
- If you or someone you know is using opioids recreationally, carry naloxone. It’s safe, easy to use, and can bring someone back from the brink.
- If you’ve been clean for a while and think about using again - don’t. Your tolerance is gone. Your risk is sky-high.
- Treatment works. Buprenorphine, methadone, and counseling can help you rebuild your life. You don’t have to quit cold turkey.
Opioids aren’t evil. They’re powerful tools. But like any tool, they can hurt as much as they help. Understanding tolerance, dependence, and overdose isn’t about fear. It’s about respect - for the drug, for your body, and for life.
Can you become dependent on opioids even if you take them as prescribed?
Yes. Physical dependence is a normal biological response to prolonged opioid use, even when taken exactly as directed. It doesn’t mean you’re addicted. But it does mean stopping suddenly can cause withdrawal symptoms like nausea, sweating, and anxiety. That’s why doctors taper doses slowly. Dependence is not a moral failure - it’s a physiological outcome.
Why do people overdose after being clean for months?
When someone stops using opioids, their body gradually loses tolerance - especially to the respiratory-depressing effects. But cravings and habits don’t disappear. If they use their old dose after weeks or months of abstinence, their body can’t handle it. This is why relapse is the leading cause of fatal overdose. Many people who die from opioids had previously completed treatment.
Is buprenorphine safer than other opioids?
Yes. Buprenorphine is a partial opioid agonist, meaning it activates receptors enough to reduce cravings and withdrawal, but not enough to cause dangerous respiratory depression. It has a ceiling effect - after a certain dose, it doesn’t get stronger. This makes it far less likely to cause fatal overdose compared to full agonists like fentanyl, oxycodone, or heroin. It’s now the cornerstone of Medication-Assisted Treatment.
Can naloxone reverse any opioid overdose?
Naloxone works on all opioids - including fentanyl, heroin, oxycodone, and methadone. It blocks opioid receptors and can bring someone back to breathing within minutes. But because fentanyl is so potent, sometimes multiple doses are needed. Naloxone is safe to use even if you’re unsure if opioids are involved. If someone is unresponsive and breathing slowly or not at all, give naloxone and call emergency services immediately.
Are prescription opioids safer than street drugs?
Prescription opioids are regulated and dosed accurately - so yes, they’re safer than street drugs. But they’re not safe when misused. Taking more than prescribed, crushing pills, or combining them with alcohol or other drugs turns them into a lethal risk. And today, many fake pills sold as oxycodone or Adderall contain fentanyl. You can’t tell by looking. So even a “prescription” pill from the street can be deadly.