More than 1 in 10 adults over 80 in the U.S. take prescription sleep pills every month. That’s not just a statistic-it’s someone’s daily reality. They’re not lazy. They’re exhausted. But what happens when the pill becomes the only thing standing between them and a sleepless night? The truth is, sleep medications aren’t a long-term fix. They’re a temporary bandage on a wound that needs real healing.
How Sleep Medications Actually Work
Sleep pills don’t make you tired. They slow down your brain. Most of them-whether they’re benzodiazepines like lorazepam or Z-drugs like zolpidem (Ambien)-boost the effect of GABA, a chemical in your brain that calms nerve activity. It’s like hitting the brakes on your nervous system. That’s why you feel drowsy. But that same braking effect doesn’t just turn off your thoughts-it can turn off your coordination, your memory, and even your ability to wake up safely.
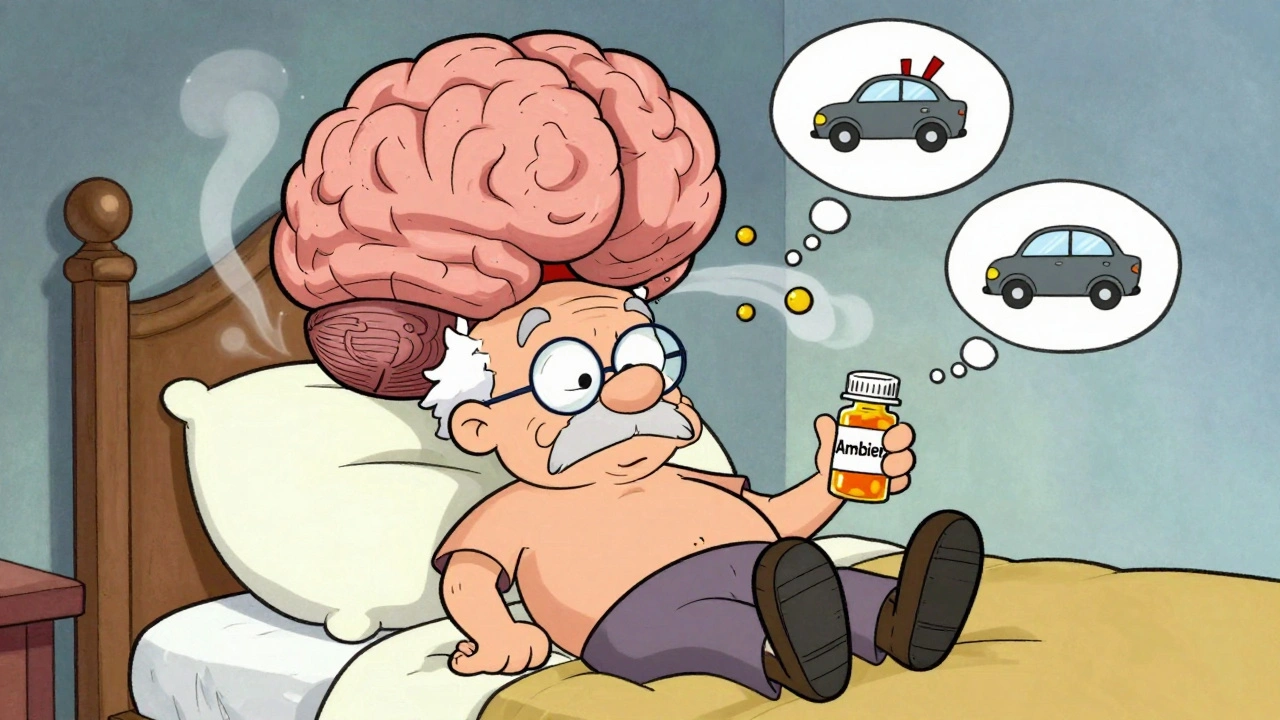
There are different types. Benzodiazepines have been around since the 1970s. They work fast and last longer, but they’re also more likely to cause dependence. Z-drugs like Lunesta and Sonata were designed to be safer. They target only specific GABA receptors, so they’re supposed to cause less daytime grogginess. But here’s the catch: studies show they’re not much better than older drugs when used for more than a few weeks. And they come with their own dangers-like sleepwalking, sleep-driving, or even making phone calls while fully asleep, with no memory of it the next day.
Then there are the off-label options. Doctors sometimes prescribe antidepressants like trazodone or doxepin for sleep. They’re cheaper, but trazodone can cause a painful, prolonged erection (priapism), and doxepin can affect your heart rhythm at higher doses. Even OTC sleep aids like Benadryl aren’t harmless. They’re antihistamines, and long-term use is linked to a 54% higher risk of dementia, according to a major study in JAMA Internal Medicine.
The Hidden Risks: Dependence, Tolerance, and Withdrawal
Dependence doesn’t mean addiction. It means your body gets used to the drug. You need it to feel normal. And when you stop, your brain doesn’t know how to sleep without it. That’s called rebound insomnia. It’s not just a bad night-it’s three or four nights of worse sleep than before you ever took the pill. Many people go back to the medication because they think, “I can’t function without this.” But the truth is, they’re not sleeping better. They’re just avoiding the crash.
Studies show up to 33% of people using benzodiazepines regularly for more than six weeks become dependent. Even Z-drugs, which are marketed as safer, have a 5-10% dependence rate. The FDA issued a boxed warning for zolpidem in 2019 after reports of people driving while asleep. The recommended dose for women was cut in half-from 10mg to 5mg-because their bodies process the drug slower. That’s not a small detail. That’s a life-or-death adjustment.
Withdrawal isn’t just about trouble sleeping. It can mean anxiety, nausea, tremors, and in rare cases, seizures. That’s why doctors recommend tapering off slowly-cutting the dose by 25% every two weeks. But here’s the problem: 40% of people who try to quit need extra help. Many don’t get it.
Why Older Adults Are at Higher Risk
If you’re over 65, taking sleep meds is like walking a tightrope. The American Geriatrics Society says these drugs should be avoided entirely in older adults. Why? Because your body changes. Your liver processes drugs slower. Your balance weakens. A single night of next-day drowsiness can mean a fall-and a broken hip. Studies show sleep medications increase fall risk by 50-60% in seniors. Fractures go up by 20-30%. And once you break a hip at 75, your chance of dying within a year jumps dramatically.
And it’s not just physical. Anticholinergic drugs-like diphenhydramine in Unisom-block a brain chemical needed for memory. Long-term use is tied to cognitive decline. For someone already worried about forgetting names or losing their keys, adding a nightly sleep pill might be the last thing they need.

The Real Solution: CBT-I
There’s a treatment that works better than any pill. It’s called Cognitive Behavioral Therapy for Insomnia, or CBT-I. It’s not a magic trick. It’s a structured program that teaches you how to retrain your brain and body to sleep naturally. It doesn’t involve chemicals. It doesn’t cause hangovers. And it lasts.
Research shows CBT-I helps 70-80% of people with chronic insomnia. That’s higher than any medication. And the benefits stick. Five years later, people who did CBT-I are still sleeping better. People who took pills? They’re back to square one-or worse.
CBT-I works by fixing the habits that keep you awake. It teaches you to associate your bed with sleep, not stress. It helps you stop racing thoughts at night. It resets your internal clock. And it’s not as scary as it sounds. Most programs last 6-8 weeks. You might see a therapist, use an app, or follow a guided program online.
One big hurdle? It takes effort. You have to stick with it. You can’t just pop a pill and forget about it. But the payoff is real. A WebMD survey found 78% of people who tried CBT-I had better long-term results than with medication. Even though 65% found the first few weeks hard, almost all said it was worth it.
New Alternatives: Digital Therapies and Emerging Drugs
Technology is catching up. In 2020, the FDA approved the first digital therapeutic for insomnia: Somryst. It’s a prescription app that delivers full CBT-I through your phone. Clinical trials showed 60% of users achieved remission-meaning they stopped meeting the clinical definition of insomnia. No pills. No side effects. Just behavioral change, delivered digitally.
Then there’s Quviviq (daridorexant), a new class of drug approved in 2022. Instead of sedating your brain, it blocks orexin-the chemical that keeps you awake. It helps you fall asleep and stay asleep, but with far less next-day grogginess than zolpidem. In trials, users reported 47% less impairment the next morning. That’s a game-changer for people who drive, work shifts, or care for children.
Even natural options are improving. Melatonin supplements are popular, and while they don’t work for everyone, they’re safe for short-term use. No dependence. No hangover. Just a gentle nudge to your body’s natural clock. But don’t expect miracles. Melatonin helps with circadian rhythm issues-like jet lag or shift work-not chronic insomnia.
When Medication Might Still Make Sense
Let’s be honest: sometimes, a pill is necessary. If you’re dealing with acute stress-like a death in the family, a divorce, or a major surgery-a short course of sleep medication can help you get through the worst of it. But it should never be the only tool. It should be paired with CBT-I from day one.
Some people with severe depression or PTSD may need medication to stabilize their sleep enough to even begin therapy. That’s where the real art of medicine comes in: knowing when to use a tool, and when to let go of it.
The key is intention. If you’re taking a pill because you’re scared you won’t sleep, you’re already in danger. If you’re taking it because your doctor said, “Let’s try this for two weeks while we start CBT-I,” you’re on the right path.
What to Do If You’re Already on Sleep Medication
If you’ve been taking sleep meds for more than a month, here’s what to do next:
- Don’t quit cold turkey. Sudden withdrawal can make sleep worse and trigger anxiety or seizures.
- Talk to your doctor about tapering. A 25% reduction every two weeks is the standard. Ask for a plan.
- Start CBT-I now. Even if you’re still on the pill, begin behavioral therapy. It’ll make quitting easier.
- Track your sleep. Use a simple journal or app. Note how long it takes to fall asleep, how many times you wake up, and how you feel in the morning.
- Avoid alcohol. Mixing sleep meds with alcohol increases overdose risk by 300%.
Many people think they’re stuck. They’re not. One user on Reddit wrote: “After six months of nightly Ambien, I tried to quit. Couldn’t sleep for three nights. I went back. Then I started CBT-I. Three months later, I’m off the pill and sleeping better than I have in ten years.”
Final Thoughts: Sleep Isn’t a Problem to Be Fixed-It’s a Habit to Be Rebuilt
Sleep isn’t something you can drug yourself into. It’s something you return to. Your body knows how to sleep. It’s just been scared off by stress, bad habits, and the false promise of a pill that works tonight but steals your tomorrow.
The best sleep aid you have is your own brain. And with the right tools, you can retrain it. No prescription needed. No side effects. Just time, patience, and a willingness to change.
Can sleep medications cause memory problems?
Yes. Many sleep medications, especially benzodiazepines and OTC antihistamines like diphenhydramine, interfere with memory formation. Long-term use of these drugs is linked to a higher risk of dementia. Even short-term use can cause next-day confusion, forgetfulness, and difficulty concentrating. The FDA has issued warnings about this for several Z-drugs, including zolpidem.
Is it safe to take sleep meds every night?
No. Clinical guidelines from the American Academy of Sleep Medicine recommend sleep medications only for short-term use-typically 2 to 5 weeks. Taking them nightly for months or years increases the risk of dependence, tolerance, and dangerous side effects like sleepwalking, falls, and cognitive decline. They’re not meant to be a permanent solution.
What’s the safest sleep aid for older adults?
The safest option for older adults is non-drug treatment: CBT-I. The American Geriatrics Society’s Beers Criteria strongly advises against all prescription sleep medications for seniors due to high risks of falls, fractures, and confusion. If medication is absolutely necessary, low-dose doxepin (3mg) may be considered under close supervision-but only after trying behavioral methods first.
Can I become addicted to melatonin?
No. Melatonin is a hormone your body naturally produces. Supplementing it doesn’t cause dependence or withdrawal. However, it’s not a cure-all. It works best for circadian rhythm issues-like jet lag or delayed sleep phase-not for chronic insomnia. Taking too much can cause drowsiness, headaches, or nausea. Stick to 0.5-3mg, taken 1-2 hours before bed.
How long does it take for CBT-I to work?
Most people start seeing improvements in 2-4 weeks. Full results usually take 6-8 weeks. It’s not instant, but the changes are lasting. Unlike pills, CBT-I doesn’t wear off. Studies show people who complete CBT-I maintain better sleep for years afterward. The hardest part is sticking with it during the first few weeks when sleep might get worse before it gets better.
If you’re tired of relying on pills to sleep, you’re not alone. And you’re not broken. Your body just needs the right support to remember how to rest. Start small. Talk to your doctor. Try a CBT-I app. Give yourself permission to heal without a prescription.