Think of the worst stomach pain you've ever felt, and then imagine living with it—on and off, sometimes daily—for years. That's a glimpse into life with Inflammatory Bowel Disease (IBD), a label covering two heavy-hitter conditions: Crohn's disease and ulcerative colitis. With treatments often falling short—leaving many stuck on endless meds or multiple bathroom trips—new solutions like Baricitinib are getting noticed. And yeah, there's hype, but there's also real science backing it. So, what's all the fuss about, and does this drug live up to its buzz?
How Baricitinib Fits Into the IBD Puzzle
Baricitinib isn’t new—it’s been a staple for rheumatoid arthritis and, more recently, hit the headlines for its role in calming immune storms in severe COVID-19 cases. What’s fresh is its entry into the IBD scene. Baricitinib belongs to a family called JAK inhibitors, which might sound like a bad sci-fi villain but is actually a group of drugs that interrupt signals promoting inflammation. Here’s how it plays out for people with IBD: while most standard meds (think steroids or immune suppressants) try to tone down your immune system, JAK inhibitors step into the cell’s command center, flipping switches off before the full alarm goes off.
Why is this a big deal? Crohn’s and colitis aren’t just gut issues—they’re the result of the immune system deciding your intestinal lining needs attacking. When this happens constantly, you get pain, diarrhea, fatigue, and—in severe cases—life-threatening complications. A lot of patients find their bodies adapt to older drugs or get hammered by side effects, leaving nothing but surgery as a last stop. Enter Baricitinib: not a miracle, but a targeted way to intercept inflammation at the source.
Here’s some real talk: researchers saw Baricitinib curb the activity of the JAK1 and JAK2 enzymes responsible for sending ‘inflammation’ messages in the gut. Instead of a broad immune system wipeout like steroids cause, Baricitinib offers precision. It slows the destructive, constant simmer of immune cells attacking the colon, letting tissues cool off and heal. As of this year, multiple phase 2 trials are showing clear drops in disease activity, with some patients—even those failing other treatments—going into remission within months. Not bad for a pill taken once a day.
What Do the Numbers Say? Real Data from Clinical Research
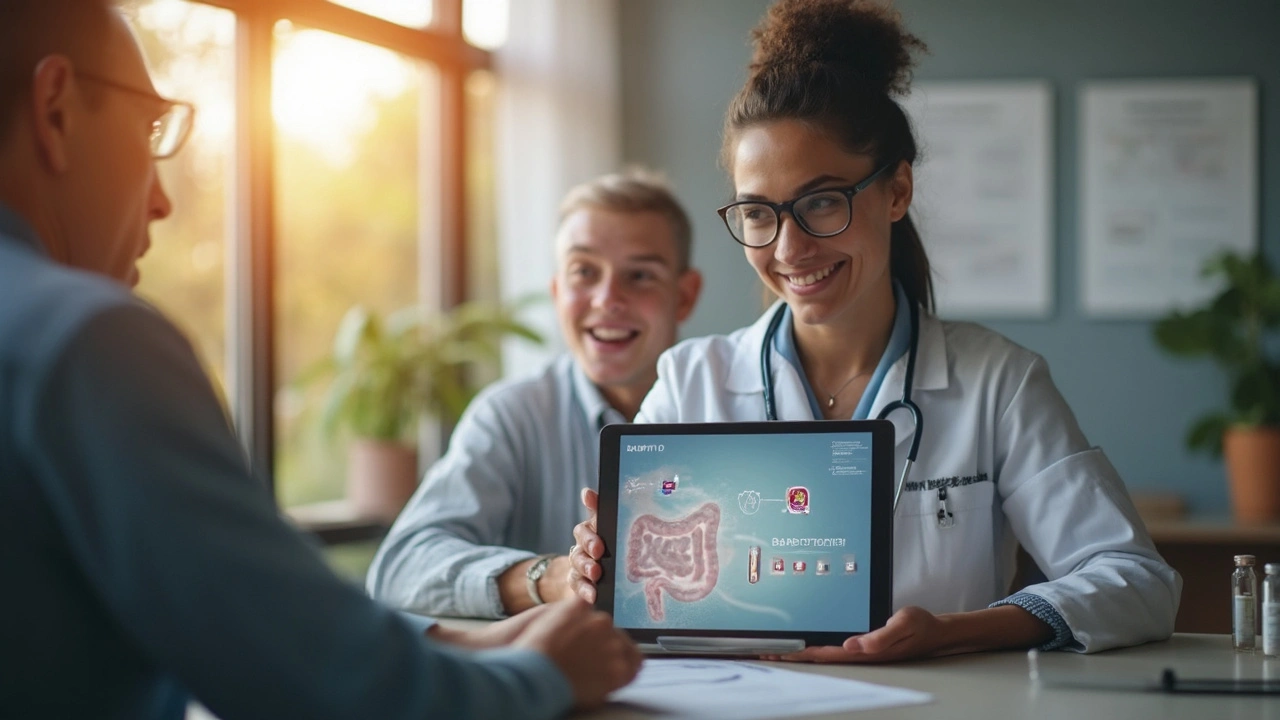
Let’s cut the sales pitch. What matters most is whether Baricitinib works for ordinary people, not just on paper. According to a 2024 multicenter trial funded in part by Eli Lilly & Co. (yep, the drugmaker), researchers followed 225 adults with moderate to severe ulcerative colitis who hadn’t gotten better with standard drugs. After 12 weeks, about 38% of folks on Baricitinib went into clinical remission. Now, 38% might not sound like a blockbuster, but compare this with just 12% in the placebo group. When you’ve bounced off multiple meds, that’s a big swing.
Crohn’s disease, the trickier of the two, saw numbers not quite as robust but still hopeful. Ongoing studies in Europe and North America point to about 30% achieving significant symptom reduction after three months. And here’s where it gets even more interesting: some patients who had no luck with older biologics (like infliximab or adalimumab) found Baricitinib got their gut back under control. These aren’t people who flinch at a little discomfort—they’re folks who’ve been through it all.
Before you get visions of never needing a bathroom map again, remember, Baricitinib isn’t perfect. It’s not a quick fix, and some people don’t respond at all. There are also safety flags (we’ll get into that next), but here’s a snapshot of reported improvements for ulcerative colitis after 12 weeks:
| Outcome | Baricitinib Group | Placebo Group |
|---|---|---|
| Clinical remission (no symptoms) | 38% | 12% |
| Endoscopic healing (no visible ulcers) | 24% | 9% |
| Sustained symptom relief | 46% | 18% |
| Adverse events reported | 21% | 13% |
This table lines up what patients in the trial actually experienced. Sure, adverse events tick up a bit, but symptom relief and remission jump by double or triple the rate over a sugar pill. The fact endoscopic healing appears in almost a quarter of cases? That’s real tissue repair, not just feeling better for a day or two.

Key Benefits and Daily Life — What Changes with Baricitinib?
Living with Inflammatory Bowel Disease is more than managing symptoms; it’s about clawing back pieces of normal life, whether that means taking your kids to soccer or just daring to commute without constant bathroom anxiety. Here’s what Baricitinib is showing so far:
- No needles: It’s a pill taken by mouth, not an injection or IV, which means less dread and no trips to infusion clinics. Huge for anyone with needle phobia (or, honestly, a busy life).
- Fast onset: Some users report changes in a matter of weeks. That means less time juggling pain, fatigue, and an unpredictable schedule.
- Works after other drugs fail: People who’ve cycled through biologics (many with harsh side effects) have seen ‘firsts’ in years—like sleeping through the night or eating out worry-free—once Baricitinib clicked.
- Easier dose adjustments: Doctors can adjust the pill more simply than with long-lasting injectables, so if you have side effects, they can pull back without waiting months.
- Fewer restrictions: So far, it plays nice with most foods and isn’t tripped up by dairy or caffeine (though always double-check if you’re a coffee junkie or have specific case quirks).
Life tips you won't find in a pamphlet: If Baricitinib is on your radar, keep a daily symptom notebook—or use an app—to track changes. Your doc needs real-life feedback on energy, sleep, bathroom trips, and unexpected boosts or flares. Cats (like my dude Nimbus) can’t rate their own gut, but you can. Also, consider joining an IBD support group online; people talk about things your GI doctor may never mention, like how certain foods mess with the med or how to time it around work shifts.
On the cost front, things get sticky. Since Baricitinib isn’t officially approved for IBD everywhere yet (as of June 2025, it’s been fast-tracked in the U.S. and U.K., awaiting broader insurance coverage), expect your healthcare team to chase down prior authorizations. Pro tip: document every treatment you’ve tried—insurers want proof you’ve exhausted other options before they pay up. If you’re in a pinch, look out for patient assistance programs through hospital social workers or nonprofit groups.
Oh, and side note for anyone juggling more than one health problem: Baricitinib might interact with meds that affect your immune system even further. For those prone to infections (which, let’s face it, is most of us in flare-ups), check with your doctor about vaccinations first. And don’t stop other meds cold-turkey—always consult before making changes, even if you start to feel like your old self again.
Risks, Side Effects, and What to Watch For
No drug is risk-free, especially one that messes with your immune signals. While Baricitinib offers a new path for a lot of people, it does ask for frequent blood tests—think of them as the early warning system for trouble. The biggies? Higher risk of infections (from annoying colds all the way to serious stuff like shingles or serious lung bugs), slightly increased chance of blood clots, and, in rare cases, impacts on cholesterol or liver enzymes. If you’ve had heart or clotting issues before, flag this up straight away when talking with your GI or primary doc.
The 2023-2024 trials reported that—while most side effects were mild (like headaches or cold symptoms)—around 1 out of every 50 Baricitinib users saw blood clots serious enough to need extra medicine or monitoring. Goes without saying, but don’t mess around: any weird leg pain, chest pain, or sudden swelling, get checked out right away. The higher infection risk is also real, especially during the first few months as your immune system adjusts. Simple tips: avoid anyone visibly sick, keep a travel-sized hand sanitizer, and stay up to date on vaccines (especially for pneumonia and flu).
If you’re prone to anxiety about side effects (guilty as charged), starting a new med like this is nerve-wracking. It helps to set up a calendar reminder for your lab checks, and don’t skip your follow-ups. A less talked-about bonus: Baricitinib doesn’t tend to trigger weight gain or sleep issues as much as steroids do, which, honestly, makes a difference when you’re already tired of feeling out of sorts.
One practical worry patients share: what about long-term damage? As of mid-2025, no evidence points to Baricitinib causing permanent organ damage in used doses for IBD. Still, all the experts demand careful monitoring, especially for folks with other chronic illness or elderly patients. Remember, the goal is to halt your inflammation without generating bigger problems down the line.
As with anything new, talk to your medical team, not just social media. They’ll tailor advice based on your risks, and sometimes even suggest backup plans if Baricitinib ends up not being your golden ticket. And hey, if you’re a parent of a teen with IBD, most studies right now are on adults, but youth trials are underway—expect more news over the next year or two.