Don’t Assume Your Prescription Is Covered
You’re prescribed a new medication. It’s essential. You pick it up at the pharmacy, hand over your card, and get hit with a bill that’s way higher than expected. This happens to thousands of people every year-not because they made a mistake, but because they never asked the right questions about their insurance.
Prescription drug coverage isn’t a simple yes or no. It’s a maze of tiers, copays, deductibles, prior authorizations, and pharmacy networks. Even if your plan says it covers prescriptions, that doesn’t mean your prescriptions are covered at a price you can afford.
According to CMS data, 63% of people enrolled in Marketplace plans in 2022 didn’t check if their specific drugs were covered until after they signed up. By then, it was too late. Nearly 3 in 10 had to switch plans the next year just to get their meds at a reasonable cost.
What’s in Your Formulary?
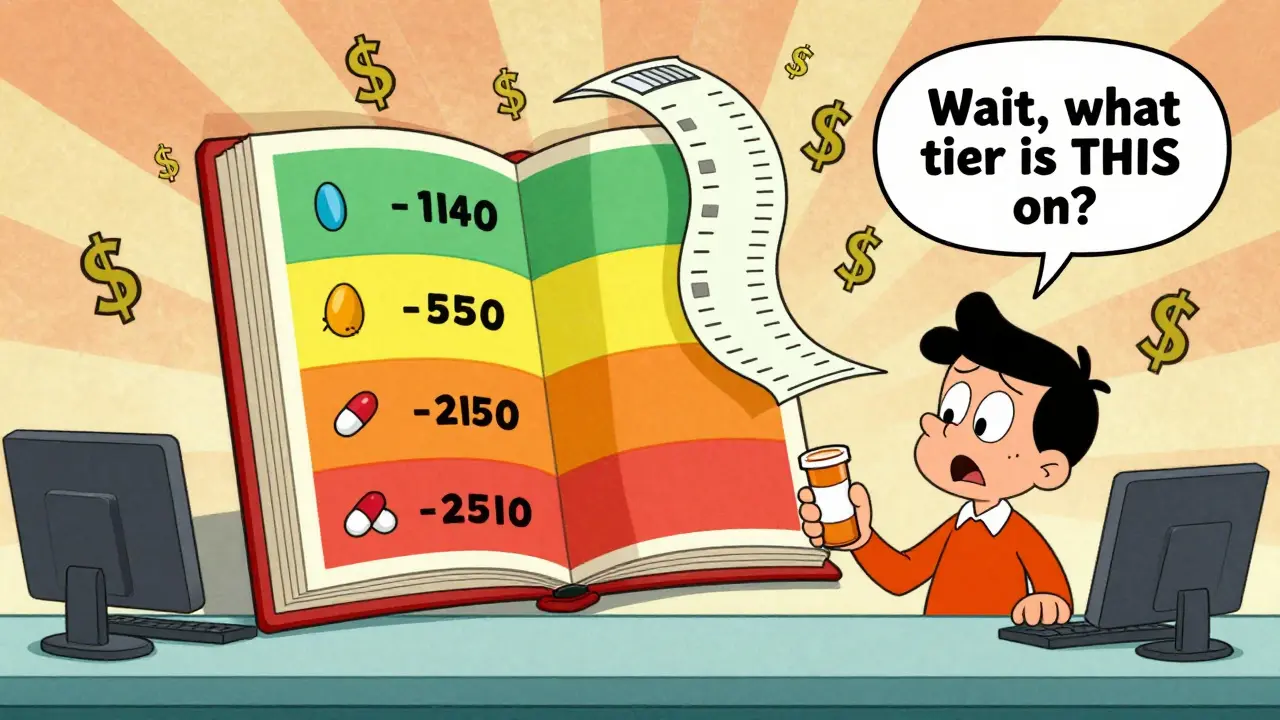
Your plan’s formulary is the official list of drugs it covers. But here’s the catch: not all drugs are treated the same. Most plans organize drugs into four tiers, each with a different cost to you.
- Tier 1: Generic drugs - Usually under $10 per prescription. These are the cheapest and most commonly covered.
- Tier 2: Preferred brand-name drugs - Around $40. These are brand-name medications your plan has negotiated lower prices for.
- Tier 3: Non-preferred brand-name drugs - Often $100 or more. These are brand-name drugs your plan doesn’t push, usually because cheaper alternatives exist.
- Tier 4: Specialty drugs - These can cost hundreds or even thousands. You might pay 25-33% coinsurance. For a $5,000 monthly drug, that’s $1,250 out of pocket.
Just because your drug is on the formulary doesn’t mean it’s in the right tier. A drug you’ve been taking for years might suddenly move to Tier 3 or get removed entirely. Always verify the tier-not just the presence-of your medication.
How Much Will You Pay Before Coverage Starts?
Many plans have a deductible for prescriptions. That means you pay 100% of your drug costs until you hit that number.
On Bronze Marketplace plans, the average prescription deductible is $6,000. That’s not a typo. If you need a $1,200 monthly insulin shot, you’d pay $14,400 in a year before your insurance kicks in. That’s impossible for most people.
Gold and Platinum plans have much lower deductibles-sometimes as low as $150. If you take multiple prescriptions, paying a higher monthly premium might save you thousands annually. CMS modeling shows someone on 12 maintenance medications saves $1,842 per year on a Gold plan versus a Bronze one.
Ask: “What’s the prescription deductible? Is it separate from my medical deductible?” Many plans combine them. Others keep them separate. That changes everything.
Are My Specific Drugs Covered?
This is the most important question. Not “Do you cover prescriptions?” but “Do you cover my prescriptions?”
Use your plan’s online tool. Enter your exact drug names, dosages, and frequency. Don’t guess. Don’t rely on what your doctor says. Doctors don’t know your insurance’s formulary.
For example: One user on Reddit thought their $4,200/month specialty drug was covered under Tier 4. Their Silver plan had a $500 copay maximum. They got billed $3,700 at the pharmacy. No one warned them.
Medicare Part D beneficiaries face the same issue. In 2023, 32% switched plans because their meds weren’t covered as expected. The biggest surprise? Prior authorization requirements. Nearly 60% of those who switched cited unexpected prior auth rules as their reason.
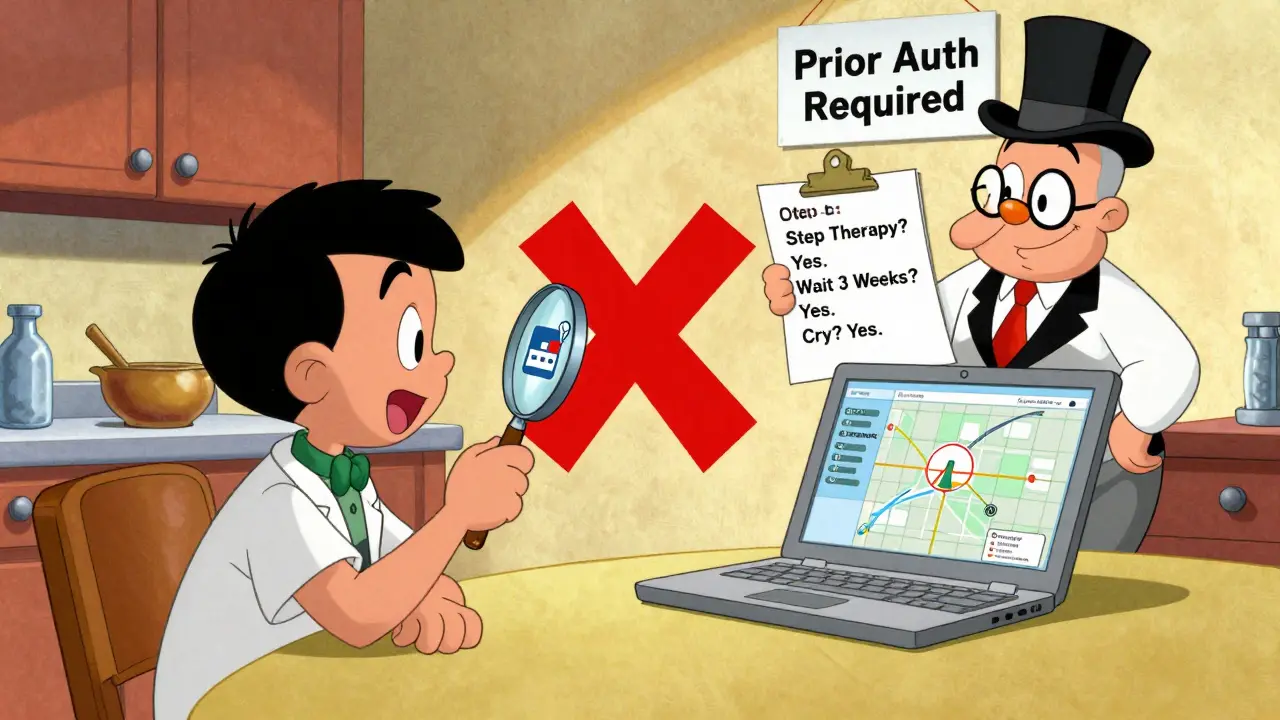
Do I Need Prior Authorization or Step Therapy?
Prior authorization means your doctor has to get approval from your insurer before the drug is covered. It’s common for specialty drugs, high-cost brand names, or drugs with cheaper alternatives.
Step therapy means you have to try a cheaper drug first-often one that doesn’t work as well for you-before your plan will pay for the one your doctor prescribed.
For chronic conditions like rheumatoid arthritis, multiple sclerosis, or diabetes, step therapy can delay effective treatment. One study found 37% of Marketplace plans use step therapy for specialty drugs. Ask your insurer: “Does this drug require prior authorization or step therapy?”
If you’re denied, you can appeal. But that takes time. If you’re already running low on meds, you can’t wait weeks.
Which Pharmacies Are In-Network?
Your plan might cover your drug-but only if you fill it at a specific pharmacy. Around 78% of Marketplace plans restrict coverage to in-network pharmacies.
Out-of-network pharmacies can cost 37% more. That’s not just a little extra. For a $200 monthly drug, that’s $74 extra per month. $888 a year.
Check your plan’s pharmacy network. Look for your local CVS, Walgreens, or independent pharmacy. Call them. Ask: “Do you accept [Plan Name]?” Don’t trust the website. Networks change.
Medicare Advantage plans are especially strict. 68% use tiered pharmacy networks. Standalone Part D plans are slightly more flexible, but still have limits.
What’s the Out-of-Pocket Maximum?
This is the most you’ll pay in a year for covered services-including prescriptions. After you hit it, your plan pays 100%.
On Bronze plans, the max is $9,450. On Platinum plans, it’s $3,050. If you take expensive drugs, a higher premium with a lower out-of-pocket max is often smarter.
Example: Someone on a $2,500/month specialty drug would hit the Bronze plan’s max after paying $9,450. That’s just four months of meds. After that, they’re covered. But those first four months could cost them $10,000. A Platinum plan with a $3,050 max? They hit it after just one month.
Ask: “What’s the total out-of-pocket maximum for prescriptions? Is it combined with medical costs?”
How Does Medicare Part D Work?
If you’re on Medicare, you have two choices: standalone Part D or a Medicare Advantage plan with drug coverage.
Standalone Part D plans let you pick any doctor and hospital, but you pay extra for drug coverage. In 2023, the average monthly premium was $34.70, and 83% had a deductible.
Medicare Advantage plans bundle medical and drug coverage. Premiums are often lower, but pharmacy networks are tighter. 68% use tiered networks versus 42% of standalone Part D plans.
Here’s what’s changing in 2025: The “donut hole” is disappearing. You’ll pay 25% of drug costs until you hit $8,000 total spending, then catastrophic coverage kicks in. Plus, insulin will cost no more than $35 per month.
Also, starting in 2025, your total out-of-pocket drug costs will be capped at $2,000 per year. That’s a game-changer for people on expensive medications.
When Should You Review Your Coverage?
Open enrollment is your only chance to switch plans without a qualifying life event.
- Marketplace plans: November 1 to January 15. Use HealthCare.gov’s plan comparison tool. Enter up to 15 medications and three pharmacies.
- Medicare Part D: October 15 to December 7. Use Medicare.gov’s Plan Finder. Enter drugs by NDC code-not brand name-for accuracy.
Don’t wait until your prescription runs out. Spend 20 minutes now. People who do save an average of $1,147 per year.
What to Do If Your Drug Isn’t Covered
If your medication isn’t on the formulary, or it’s in a high tier:
- Ask your doctor for a generic or preferred brand alternative.
- Request a formulary exception. Submit a letter from your doctor explaining why the drug is medically necessary.
- Check patient assistance programs. Drug manufacturers often offer discounts or free meds to low-income patients.
- Use GoodRx or SingleCare for cash prices. Sometimes they’re cheaper than your insurance copay.
One user saved $8,400 a year by switching to a Gold plan after checking her insulin coverage. The $200 higher premium was worth it. She didn’t guess. She checked.
Final Checklist Before You Enroll
Before you sign up for any plan, answer these five questions:
- Is my exact medication on the formulary, and what tier is it in?
- What’s the prescription deductible? Is it separate from my medical deductible?
- Do I need prior authorization or step therapy for my drugs?
- Is my pharmacy in-network? What’s the cost difference if I go out-of-network?
- What’s the out-of-pocket maximum for prescriptions?
If you can’t answer all five, don’t enroll. Wait. Call your insurer. Ask for a written copy of the formulary. Save it.
Prescription drugs aren’t optional. For millions, they’re life or death. Don’t let insurance paperwork decide your health.
Are all prescription drugs covered by insurance?
No. Insurance plans only cover drugs on their formulary, and even then, coverage varies by tier. Some drugs require prior authorization, step therapy, or are excluded entirely. Always check your specific medications before enrolling.
What if my drug isn’t on the formulary?
You can request a formulary exception by submitting a letter from your doctor explaining why the drug is medically necessary. You can also ask your doctor for an alternative drug on the formulary. Some manufacturers offer patient assistance programs to help with costs.
How do I find out if my pharmacy is in-network?
Visit your insurer’s website and search their pharmacy network directory. Call your pharmacy directly and ask if they accept your plan. Don’t rely on online tools alone-networks change frequently.
What’s the difference between a copay and coinsurance for prescriptions?
A copay is a fixed amount you pay per prescription-like $10 or $40. Coinsurance is a percentage of the drug’s cost-like 25% or 33%. Specialty drugs usually have coinsurance, which can make them much more expensive than drugs with a flat copay.
When can I change my prescription drug plan?
You can change during Open Enrollment: November 1 to January 15 for Marketplace plans, and October 15 to December 7 for Medicare Part D. Outside those windows, you can only switch if you have a qualifying life event, like moving or losing other coverage.
Will Medicare’s new $2,000 cap affect my drug costs in 2025?
Yes. Starting in 2025, Medicare Part D beneficiaries will pay no more than $2,000 out of pocket for prescription drugs each year. This cap applies to all drugs, including specialty medications. It also eliminates the coverage gap (donut hole) and caps insulin at $35 per month.
What’s Next?
If you’re still unsure, call your insurer’s member services. Have your drug list ready. Ask for a written copy of the formulary. Save the conversation.
Next year’s enrollment starts in November. Don’t wait until you’re out of meds to act. Take 20 minutes now. It could save you thousands.