After surgery, you’re often given short-term medications to manage pain, prevent infection, or control swelling. These drugs-like opioids, antibiotics, or anti-nausea pills-are meant to help you heal, not to be taken longer than needed. But here’s the hard truth: medication errors after surgery are more common than most people realize. According to the Joint Commission, 30% of all medication mistakes happen in surgical settings. Many of these aren’t caused by patients-they’re caused by system gaps, rushed procedures, or poor labeling. The good news? You can protect yourself by knowing what to watch for and how to speak up.
Know What You’re Taking
You won’t always get a written list of your post-op meds. Sometimes, nurses hand you a pill bottle with no instructions. Other times, you’re given an IV drip with no clear label. That’s not normal-and it’s dangerous. The Institute for Safe Medication Practices (ISMP) says every syringe, cup, or vial on the sterile field must be labeled with the drug name, concentration, and expiration time. If it’s not labeled, ask for it. If no one can label it, refuse to take it.High-alert medications like morphine, fentanyl, heparin, or insulin are especially risky. A single wrong dose can cause breathing problems, internal bleeding, or even death. Ask your nurse: “Is this the right dose for my weight and surgery type?” If they hesitate or can’t answer, pause. It’s better to wait five minutes than to risk harm.
Use Aseptic Technique-Every Time
The CDC updated its injection safety guidelines in November 2023, and the message is clear: one needle, one syringe, one patient. Even if the same nurse gives you multiple doses, they must use a fresh syringe each time. Reusing a syringe-even for the same person-can introduce bacteria into your bloodstream. This isn’t just theory. Between 2001 and 2011, 44 outbreaks of hepatitis B and C were traced back to unsafe injection practices in hospitals, affecting over 14,000 patients.After surgery, you might see a nurse draw up medicine from a multi-dose vial. That’s okay-if they use a new sterile needle and syringe each time. But if they use the same needle to draw from the vial and then inject you, that’s a violation. Don’t be afraid to say: “Can you please use a new needle?” You’re not being difficult-you’re protecting your health.
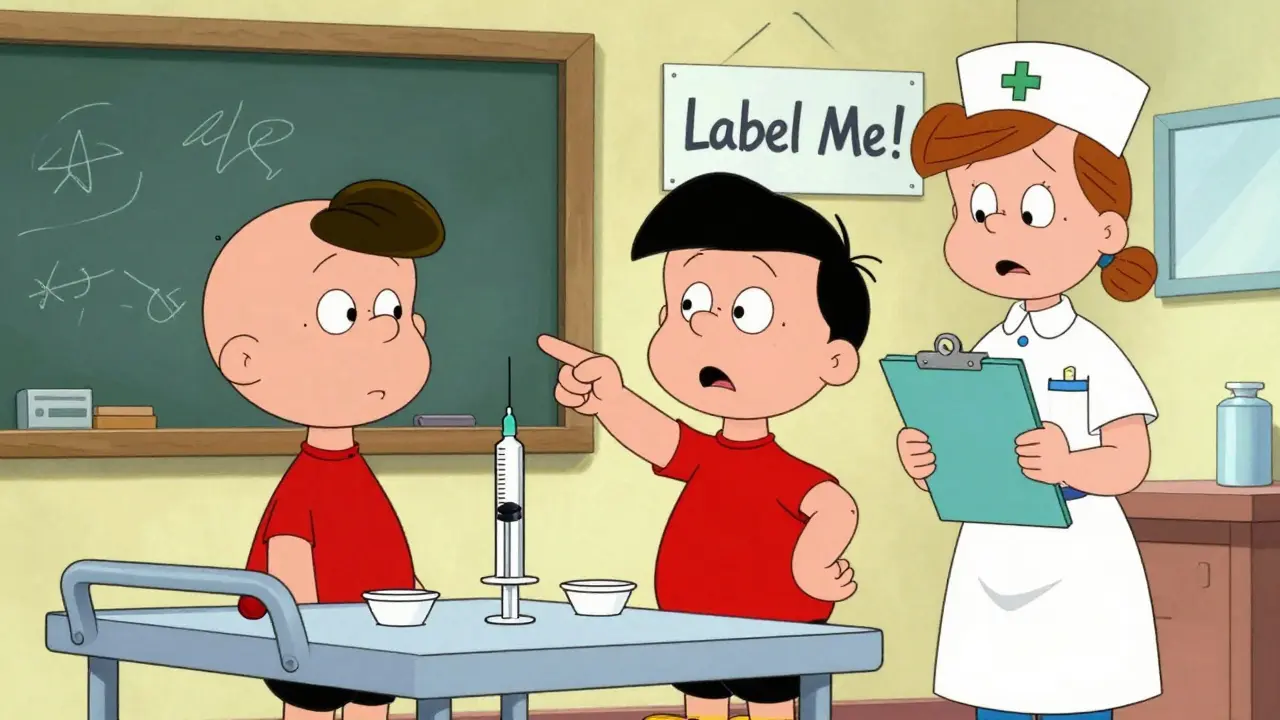
Watch for Labeling Mistakes
One of the most common causes of medication errors is unlabeled or mislabeled containers. The Association of Surgical Technologists (AST) requires that every medication on the sterile field be labeled immediately after being prepared. Yet, a 2021 AORN survey found that 41% of nurses sometimes skip labeling because they’re rushed.Here’s what to look for: If you see a syringe with just a drop of liquid and no text, or a cup with a scribbled “morphine” on it, that’s not safe. Labels must include:
- Drug name (e.g., “Fentanyl 50 mcg/mL”)
- Concentration (how strong it is)
- Expiration time (when it’s no longer safe to use)
Some facilities use color-coded labels or barcode scanners. If yours doesn’t, ask why. Facilities that implement full labeling protocols reduce medication errors by up to 47%, according to a 2022 study in the AORN Journal.
Speak Up During Verbal Orders
In the operating room and recovery area, most medication orders are given verbally-not written. A doctor says, “Give 1 mg of morphine,” and the nurse administers it. But what if they meant 0.1 mg? Or what if they said “morphine” but meant “hydromorphone”? That’s not rare. The World Health Organization found that verbal orders are 25% more likely to be misunderstood than written ones.Always insist on a “read-back.” That means the nurse repeats the order back to the doctor before giving it. Example:
Doctor: “Give 0.5 mg of hydromorphone IV.”
Nurse: “You want 0.5 mg of hydromorphone IV-correct?”
Doctor: “Yes.”
This simple step reduces errors by 55%, according to the American College of Obstetricians and Gynecologists. If the nurse doesn’t do this, ask them to. It’s not rude-it’s necessary.

Don’t Assume “It’s Just a Pill”
Many patients think the hardest part is over once they leave the hospital. But the first 72 hours after surgery are when most medication-related problems occur. You might get a prescription for opioids, and the bottle says “Take one every 6 hours as needed.” But what if you’re not in pain? Don’t take it anyway. Opioids don’t just relieve pain-they slow your breathing. Taking them when you don’t need them increases your risk of overdose.Also, never mix opioids with alcohol, sleeping pills, or anti-anxiety meds. That combination can stop your breathing. Even over-the-counter cold medicines can interact dangerously. Always check with your pharmacist before taking anything new.
Track Your Medications
Keep a simple log: write down what you took, when, and how you felt. Did you take your pain pill at 2 p.m. and feel dizzy by 4 p.m.? That’s a red flag. Did you take two pills because you thought the first didn’t work? That’s how overdoses happen.Use your phone. Set reminders. Take a photo of your pill bottle with the instructions. If you’re confused, call your surgeon’s office-not a random pharmacist or Google. Your surgical team knows your case best.
Ask About Discharge Plans
Medication reconciliation-the process of checking what you were on before surgery versus what you’re going home with-is one of the most powerful safety tools. The WHO says proper reconciliation can cut adverse drug events by 67% in surgical patients.Before you leave the hospital, ask:
- “What medications am I going home with?”
- “Which ones should I stop?”
- “Do I still need the pain pills, or can I switch to ibuprofen?”
- “When should I call if something feels wrong?”
Many patients are sent home with antibiotics they don’t need, or pain meds they’ll never use. Unnecessary drugs mean unnecessary side effects and higher risk of addiction.

Know the Warning Signs
You’re not expected to be a doctor-but you should know when something’s wrong. Call your doctor or go to the ER if you experience:- Slowed or shallow breathing
- Extreme drowsiness you can’t wake from
- Confusion or trouble speaking
- Swelling, redness, or warmth at an injection site
- Fever over 101°F after the first 24 hours
These aren’t normal. They’re signals your body is reacting badly to a medication.
What Facilities Should Be Doing
You shouldn’t have to fight for safety. Hospitals and surgery centers are required by law to prevent medication errors. The Joint Commission classifies incorrect medication administration as a “sentinel event”-meaning it’s serious enough to trigger a full investigation. In 2022, medication errors were the third most common sentinel event reported.Facilities that follow the ISMP 2022 guidelines see a 73% drop in serious errors over five years. But only 63% of ambulatory surgery centers have full protocols. Academic hospitals are better, at 87%. That gap matters. If your surgery center doesn’t label syringes, doesn’t use read-backs, or lets nurses draw meds from unlabeled vials, consider asking if they follow the latest safety standards.
Final Advice: Be Your Own Advocate
You’re not just a patient-you’re the most important member of your care team. You know your body better than anyone else. If something feels off, if a label looks wrong, if a dose seems too high-speak up. Don’t assume someone else is checking. Don’t worry about being “difficult.”Safety isn’t about rules. It’s about people paying attention. And you have the right to expect that.
Can I reuse a syringe if it’s for the same person during one surgery?
No. Even if it’s the same patient, a syringe used for incremental dosing during a procedure must be discarded immediately after the procedure ends. The CDC requires this to prevent contamination and accidental reuse. A syringe should never be left unattended on a table or cart-even for a few minutes. If you see one sitting out, ask for a new one.
What if the nurse says they’re in a hurry and skips labeling?
Say: “I understand you’re busy, but I need to know exactly what’s being given to me.” Unlabeled medications are a leading cause of errors. If they refuse to label it, ask to speak to a supervisor. You have the right to safe care. Time pressure is not an excuse for cutting corners.
Are opioids always necessary after surgery?
No. Many minor surgeries-like hernia repairs or knee arthroscopies-can be managed with acetaminophen or ibuprofen alone. Opioids are only needed for moderate to severe pain. Ask your surgeon: “Can I avoid opioids?” If they say no, ask why. Many patients get prescribed opioids out of habit, not need. Reducing opioid use lowers your risk of addiction and overdose.
How do I safely dispose of leftover pills?
Never flush pills down the toilet or throw them in the trash. Use a drug take-back program-many pharmacies and police stations offer free drop-off bins. If that’s not available, mix pills with used coffee grounds or cat litter in a sealed container before throwing them away. This prevents accidental ingestion by children or pets.
Can I take my regular medications after surgery?
Not always. Some blood thinners, diabetes meds, or herbal supplements can interfere with healing or increase bleeding risk. Always ask your surgical team which of your regular meds to stop before surgery and when to restart them. Don’t assume your usual routine is safe post-op.