When a patient switches from a brand-name drug to a generic, they often don’t realize the pills are chemically identical. But their body might react differently-not because of the medicine, but because of what they believe it is.
Why Generic Pills Feel Different
A 2025 study gave healthy volunteers a fake nasal spray labeled either as a brand-name product or a generic. Both versions had zero active ingredients. Yet those told they were taking the generic version reported more side effects-headaches, dizziness, nausea-than those told they were taking the brand. The difference? Expectations. The same thing happens in real life. When patients are switched from, say, Zoloft to sertraline, they often report new or worse side effects-even though blood tests show identical drug levels. This isn’t a failure of the generic. It’s the nocebo effect in action.The word "nocebo" comes from Latin: "I shall harm." It’s the dark twin of the placebo effect. Where placebo makes you feel better because you expect to, nocebo makes you feel worse because you expect to. And when it comes to generics, that expectation is often shaped by price, packaging, and misinformation.
Price Tells the Story
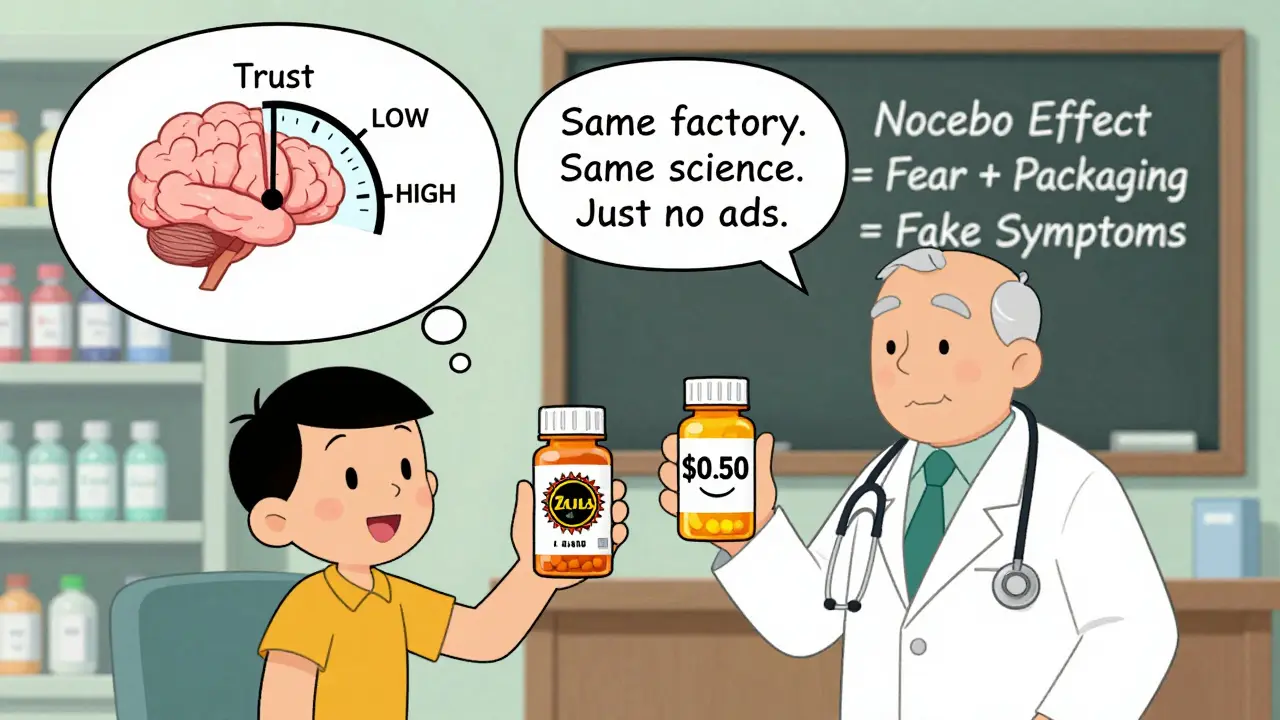
In one experiment, researchers gave people a fake anti-itch cream. One group got it in a sleek blue box labeled "Solestan® Creme." The other got the same cream in a plain orange box labeled "Imotadil-LeniPharma Creme." The cream had no active ingredient. But the people who thought they were using the expensive version reported more pain sensitivity-a known side effect. Why? Because their brains linked higher price with higher potency, and therefore, higher risk of side effects.This isn’t just about money. It’s about trust. When a pill costs $0.50 instead of $5, patients wonder: "Is this really the same?" Even when told it is, the subconscious mind doesn’t always believe it. A 2023 study in PLOS Medicine confirmed this: patients on authorized generics-medications made by the same company, in the same factory, with the exact same formula as the brand-still reported more side effects. The packaging was different. That was enough.
How Packaging and Labels Shape Perception
The shape, color, and size of a pill matter more than you think. A patient who’s been on a white, oval tablet for years might panic when switched to a blue, round one-even if it’s the same drug. In Germany, neuroscientists found that even the font on the label changed how patients reported side effects. The more clinical, impersonal, or "cheap-looking" the packaging, the more side effects patients claimed.And it’s not just the pill. The way it’s prescribed matters too. If a doctor says, "I’m switching you to a generic because it’s cheaper," the patient hears: "This is the low-quality option." But if the doctor says, "This is the exact same medicine, just without the brand name," the outcome changes. Language is powerful. Framing matters.
The Role of Media and Social Rumors
In 2017, New Zealand switched the brand of venlafaxine. Initially, adverse event reports didn’t spike. Then the media ran stories about "generic side effects." Suddenly, reports jumped 400%. The medicine hadn’t changed. The patients’ minds had.Today, Reddit threads like r/pharmacy are filled with posts like: "My doctor switched me to generic sertraline and now I can’t sleep, I’m crying all day, and I feel like I’m dying." These aren’t lies. These are real experiences-created by fear, not chemistry. The same thing happens with statins, antidepressants, blood pressure meds. When a patient hears someone else had a bad reaction, their brain starts scanning for symptoms. A headache? Must be the pill. Fatigue? Must be the pill. Even normal stress becomes "evidence."
What Doctors Can Do
The best way to fight the nocebo effect isn’t with science-it’s with communication. Here’s what works:- Don’t say "generic" unless you have to. Instead, say: "This is the same active ingredient as your old pill, just made by a different company. Studies show patients do just as well on it."
- Avoid listing every possible side effect. Saying "Some people get nausea, dizziness, or fatigue" plants the idea. Better: "Most people tolerate this well. If you notice anything unusual, we’ll figure it out together."
- Use positive framing. Instead of "This may cause headaches," say "Less than 5% of people report mild headaches, and they usually go away in a few days."
- Explain bioequivalence simply. "The FDA requires that generics deliver the same amount of medicine into your bloodstream as the brand. They’re tested on thousands of people. They’re not cheaper because they’re weaker-they’re cheaper because they don’t pay for ads or fancy packaging."
- Offer to switch back-if needed. Giving patients control reduces anxiety. Say: "If you don’t feel right after two weeks, we can go back. But let’s give it a fair shot first."
Why This Matters for Public Health
In the U.S., 90% of prescriptions are for generics. That’s a good thing. Generics save patients and the system billions. But if 38% of patients still believe generics are less effective, and if 15-22% of reported side effects after switching are due to perception-not chemistry-then we’re wasting money and harming trust.When patients stop taking their meds because they think the generic isn’t working, their blood pressure rises. Their depression returns. Their cholesterol climbs. The real harm isn’t the pill. It’s the fear.
Health systems like Kaiser Permanente now train staff to use scripted messages when switching patients: "This medicine has the same active ingredient as your previous one. It’s been approved by the FDA and works the same way. Many patients switch without any change in how they feel."
And it works. A 2022 study found that when patients were told generics save $3,172 per year-and that those savings go to better care for everyone-nocebo effects dropped by 37%. Money talks. But so does fairness.
What Patients Can Do
If you’ve switched to a generic and feel worse:- Don’t assume it’s the pill. Ask: "Could this be stress, sleep, or something else?"
- Track your symptoms for two weeks. Write down when they happen. Are they worse on certain days? After meals? When you’re tired?
- Ask your doctor: "Is this likely the medication, or could it be the nocebo effect?"
- Look up the FDA’s bioequivalence data. You’ll see the same numbers as the brand.
- Consider asking for the branded generic-same formula, same factory, just a different name. It’s still generic, but often less alarming to patients.
The Bigger Picture
The nocebo effect isn’t about gullibility. It’s about how deeply our minds shape our physical experience. Pain, fatigue, nausea-these aren’t just signals from the body. They’re signals filtered through belief, culture, fear, and past experience.Generic drugs are safe. They’re effective. They’re the backbone of modern healthcare. But until we fix how we talk about them, patients will keep suffering-not because the medicine fails, but because the story around it does.
The solution isn’t more science. It’s better storytelling. Clearer language. More trust. And the quiet, powerful reminder: your body doesn’t know the price tag. It only knows what you tell it to believe.
Do generic medications work the same as brand-name drugs?
Yes. The FDA requires that generic drugs contain the exact same active ingredient, strength, dosage form, and route of administration as the brand-name version. They must also deliver the same amount of medicine into the bloodstream at the same rate. This is called bioequivalence. Studies show that 90% of patients respond identically to generics and brands. The differences people feel are usually psychological, not chemical.
Why do some people report side effects after switching to a generic?
The most common reason is the nocebo effect. When patients expect side effects-because the pill looks different, costs less, or they heard someone else had a bad experience-their brains can trigger real physical symptoms. This isn’t "all in your head"-it’s a real biological response to belief. Studies show that even inert pills labeled as generics cause more reported side effects than identical pills labeled as brand-name.
Can the packaging of a generic drug affect how I feel?
Absolutely. Research shows that pill color, shape, size, and even the font on the label influence how people report side effects. A plain orange box labeled with a complex company name can trigger more anxiety than a sleek blue box with a familiar brand name-even if the medicine inside is identical. Packaging isn’t just marketing. It’s part of the treatment experience.
Should I ask my doctor to keep me on the brand-name drug?
If you’re stable and doing well on a generic, there’s usually no medical reason to switch back. But if you’re genuinely struggling after a switch, talk to your doctor. They can help determine whether it’s a true reaction or a nocebo effect. In some cases, switching to a "branded generic"-same formula, same factory, different name-can ease anxiety without increasing cost. Your comfort matters, and your doctor should support your concerns without judgment.
Are there any real risks with generic medications?
The risks are extremely low. Generic drugs must pass the same rigorous testing as brand-name drugs. The FDA inspects manufacturing facilities for both. The only real risk comes from miscommunication-when patients believe generics are inferior and stop taking them. That’s when health problems arise. The medicine itself is not less safe.
How can I tell if my side effects are from the drug or from my expectations?
Track your symptoms for 2-4 weeks. Note when they started, how often they occur, and what else is happening in your life (stress, sleep, diet). If symptoms appear immediately after switching and match the side effects you were warned about, it’s likely the nocebo effect. If symptoms develop gradually or don’t match the known profile, it could be something else. Talk to your doctor about your concerns-they can help you distinguish between psychological and physiological causes.