Why Reading Medication Labels Matters
Every year, thousands of people end up in emergency rooms because they took the wrong dose of medicine. Not because they were careless, but because they didn’t understand what the label actually said. A 2022 study found that 42% of adults misread liquid medication concentrations-parents of young kids made mistakes even more often. That’s not just a statistic. That’s someone giving their child six times the right dose because they thought the whole bottle was one serving.
Medication labels aren’t just paperwork. They’re your first and last line of defense against dangerous mistakes. Whether it’s a prescription pill bottle or a bottle of ibuprofen from the pharmacy shelf, the label holds the key to safe use. The FDA requires clear, standardized formats for both prescription and over-the-counter drugs, but that doesn’t mean everyone reads them the right way.
What’s on a Prescription Label
Prescription labels have a lot of information, but you only need to focus on a few critical parts:
- Your name - Always check this first. A mix-up here can be deadly.
- Medicine name - Both the brand name (like Advil) and the generic name (ibuprofen). Make sure it matches what your doctor told you.
- Dosage - This tells you how much to take. It might say “take one 200mg tablet.” That means each pill has 200 milligrams of the active ingredient.
- Directions - How often? When? With food? “Take one tablet every 6 hours as needed for pain” is clear. “Take twice daily” means morning and night, not every 12 hours if you’re awake longer.
- Expiration date - Most pharmacies set this for one year after filling, even if the bottle says it lasts longer. Expired meds can lose strength or become unsafe.
- Warnings - These are non-negotiable. “Do not drink alcohol” or “May cause drowsiness” aren’t suggestions. They’re safety rules.
For complex drugs-like cancer treatments, blood thinners, or insulin-the label might include extra notes: “Check liver function before starting” or “Take with 8 oz of water.” These aren’t filler. They’re life-saving.
What’s on an Over-the-Counter (OTC) Label
OTC labels follow the FDA’s “Drug Facts” format. It’s designed to be simple, but people still miss the most important parts. Here’s what you need to know:
- Active ingredient - This is the medicine itself. It’s listed first and in bold. If you’re taking more than one OTC product, check this section. Many cold and pain meds share the same active ingredient-like acetaminophen. Taking two with acetaminophen can cause liver damage.
- Purpose - Tells you what the medicine does. “Pain reliever,” “antihistamine,” “decongestant.” Know what you’re taking.
- Uses - What symptoms it treats. Don’t assume it works for something not listed.
- Dosage - This is the most critical part. It tells you exactly how much to take and how often. “Take 1 tablet every 4 to 6 hours.” Never exceed the maximum daily dose. For kids, it often says “based on weight” - so know your child’s weight before giving anything.
- Warnings - Again, don’t skip this. “Do not use if you have high blood pressure.” “May cause drowsiness.” “Do not give to children under 6.” These are not suggestions. They’re rules.
- Other information - Includes storage tips and inactive ingredients (like dyes or sugars) that might matter if you have allergies.
One of the biggest mistakes? Taking multiple OTC meds at once. Someone takes a cold tablet with acetaminophen, then takes a separate painkiller with acetaminophen. They don’t realize they’ve hit 3,000mg in one day-over the safe limit. The label tells you this. You just have to read it.

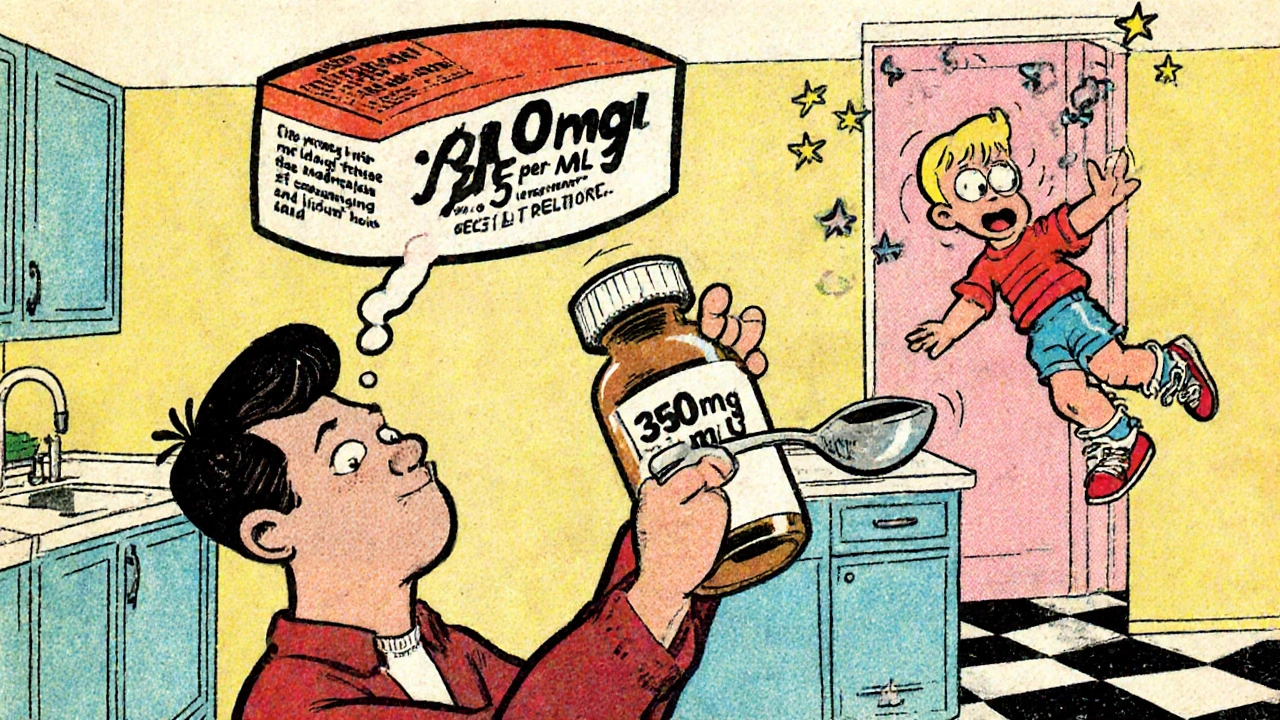
Understanding Liquid Medication Dosing
Liquid meds are where most mistakes happen. Why? Because people use kitchen spoons.
A teaspoon isn’t 5 milliliters. It can be anywhere from 2.5 to 7.3 mL. A tablespoon? Between 7 and 14.8 mL. That’s why the American Academy of Pediatrics says: never use household spoons.
Instead, use the measuring tool that came with the medicine-usually a plastic syringe or a dosing cup with milliliter (mL) markings. If it didn’t come with one, ask the pharmacist for one. They’re free.
Now, look at the concentration. It might say: “350 mg per 5 mL.” That means each mL has 70 mg. If your child needs 700 mg, you need 10 mL-not two spoonfuls. Do the math: 700 ÷ 70 = 10 mL. Use the syringe. Measure slowly. Double-check.
One Reddit user shared a story: a patient thought the whole 30 mL bottle of amoxicillin was a single dose. It wasn’t. It was six doses. That’s six times the intended amount. That’s not a typo. That’s a misunderstanding of concentration.
What You Should Never Ignore
There are three sections on every label that people skip-and pay for it:
- Warnings - 47% of people don’t read them, according to Express Scripts. But warnings like “may cause severe skin reaction” or “avoid sunlight” are critical.
- Dosage modifications - If you have kidney or liver disease, your dose might need to be lower. This is often buried in fine print on prescriptions. If you’re unsure, ask.
- Drug interactions - Some meds shouldn’t be taken with alcohol, grapefruit juice, or other drugs. For example, statins (cholesterol meds) can cause muscle damage if taken with certain antibiotics. The label will say so.
And don’t forget: if the label says “take with food,” take it with food. If it says “take on an empty stomach,” wait two hours after eating. These aren’t suggestions. They affect how well the drug works.
The Five Rights of Medication Safety
Nurses use a simple checklist called the “Five Rights” to prevent errors. You can use it too:
- Right patient - Is this medicine for you? Check your name.
- Right drug - Does the name match what your doctor prescribed?
- Right dose - Does the amount match what you were told? If it’s 500mg but you were told 250mg, call the pharmacy.
- Right route - Is it meant to be swallowed? Applied to skin? Injected? Don’t guess.
- Right time - Morning? Night? Every 8 hours? Take it when it says.
If you can’t answer all five with confidence, don’t take it. Call your pharmacist. They’re trained to help.

What’s Changing in Medication Labels
Labeling is getting better. The FDA is pushing for plain language. By 2025, high-risk drugs like insulin, opioids, and blood thinners must use simple terms: “Take one pill at bedtime” instead of “Administer 1 tablet PO at HS.”
Some pharmacies are testing QR codes on bottles. Scan it, and you get a short video showing how to use the medicine. One pilot program cut medication errors by 37%.
By 2027, you might see color-coded caps or icons on bottles: red for high-alert drugs, yellow for drowsiness risk. These aren’t science fiction-they’re coming.
What to Do If You’re Still Confused
It’s okay to not understand. You’re not alone. Here’s what to do:
- Call your pharmacist. They’re available during business hours and often after hours too.
- Ask for a printed sheet with plain-language instructions.
- Use a pill organizer with times labeled (morning, noon, night, bedtime).
- Take the bottle to your doctor’s next visit and ask: “Can you show me how to take this?”
- For kids, write the dose on the bottle with a marker. “10 mL twice daily.”
There’s no shame in asking. The real risk is guessing.
Final Reminder
Medication labels are designed to protect you. But they only work if you read them. Don’t assume. Don’t guess. Don’t rely on memory. Every time you pick up a new bottle, stop. Read it. Double-check. Ask. That one habit can keep you-and your family-safe.





