Isoniazid is one of the most important antibiotics ever developed for tuberculosis. Since it was first introduced in the 1950s, it has saved millions of lives worldwide. Today, it’s still the backbone of TB treatment in nearly every country, including the UK. But despite its effectiveness, many people don’t know how it works, what it does to the body, or why it comes with serious warnings. This isn’t just another pill. It’s a powerful drug that can prevent death-or cause serious harm if used wrong.
What is isoniazid and how does it kill TB bacteria?
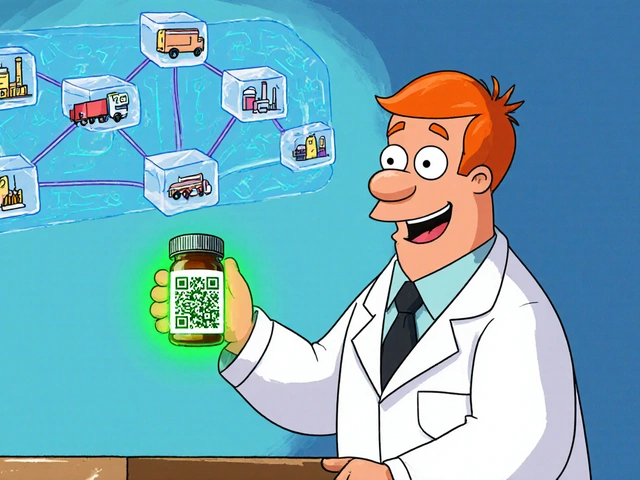
Isoniazid, often shortened to INH, is a synthetic antibiotic made specifically to target Mycobacterium tuberculosis, the bacteria that causes tuberculosis. Unlike broad-spectrum antibiotics that attack many types of bacteria, isoniazid is narrow in focus. It only works on mycobacteria, which makes it perfect for TB but useless for other infections like strep throat or pneumonia.
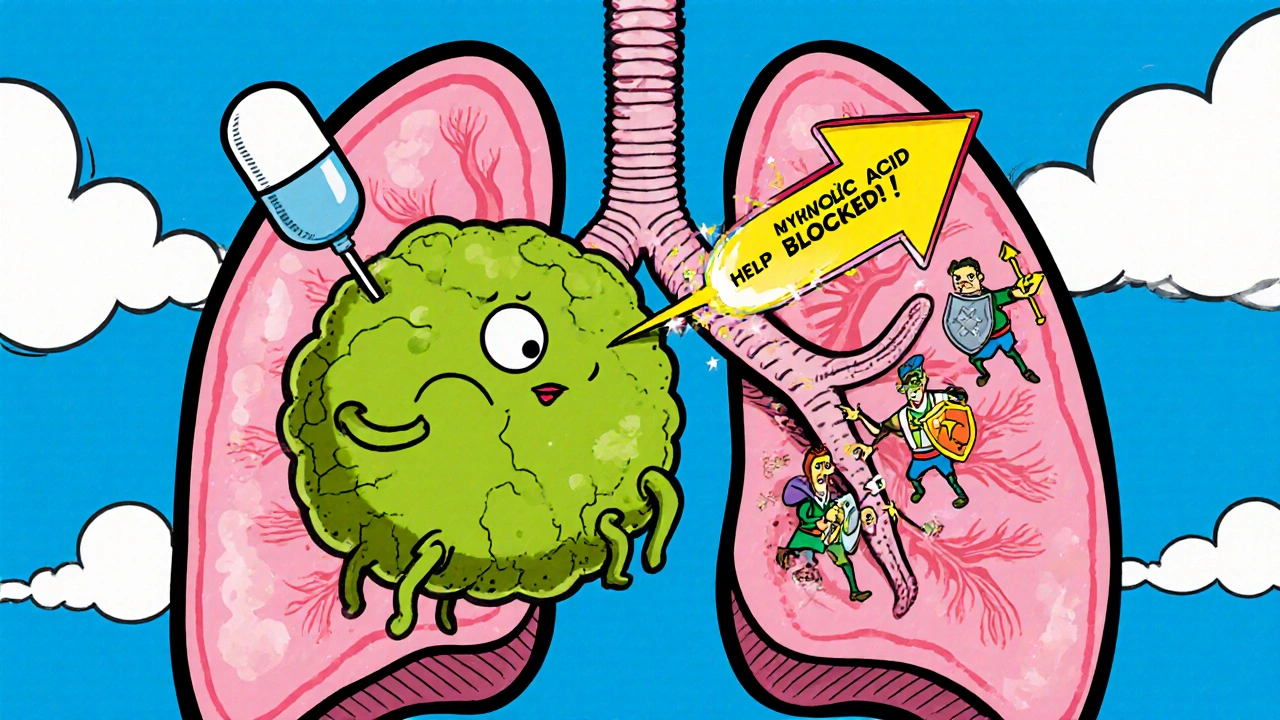
The drug works by blocking the production of mycolic acid, a fatty substance that forms the thick, waxy outer shell of TB bacteria. Without that shell, the bacteria can’t survive. They become weak, leaky, and easy for the immune system to destroy. This is why isoniazid is so effective at killing TB bacteria in the early stages of infection-even when they’re hiding deep in the lungs or lymph nodes.
It’s not just for active TB. Isoniazid is also used to treat latent TB infection, where the bacteria are present but not causing symptoms. In this case, taking isoniazid for 6 to 9 months stops the infection from becoming active later. For people with HIV or those who’ve been in close contact with someone with active TB, this preventive use can be life-saving.
Who takes isoniazid and why?
In the UK, isoniazid is most commonly prescribed in three situations:
- People diagnosed with active pulmonary TB-always combined with other drugs like rifampicin and pyrazinamide.
- Those with latent TB infection, especially if they’re at high risk of developing active disease (like healthcare workers, recent immigrants from high-TB countries, or people with weakened immune systems).
- Children exposed to TB who test positive for latent infection but show no signs of illness.
The NHS recommends isoniazid for latent TB because the risk of developing active TB within two years can be as high as 10% without treatment. With isoniazid, that risk drops to less than 1%. That’s why contact tracing for TB often includes offering isoniazid to household members-even if they feel fine.
It’s not for everyone. People with a history of liver disease, severe alcohol use, or previous allergic reactions to isoniazid are usually not prescribed it. Doctors check liver enzymes before starting and again after a few weeks to make sure the liver is handling it.
Side effects: What you might feel-and what you must report
Most people tolerate isoniazid well. But side effects happen. The most common ones are mild: nausea, upset stomach, dizziness, or a mild rash. These often go away after a few days as your body adjusts.
But some side effects are dangerous. The biggest risk is liver damage. Isoniazid can cause hepatitis, especially in people over 35, those who drink alcohol regularly, or people taking it for longer than three months. Symptoms to watch for:
- Yellowing of the skin or eyes (jaundice)
- Dark urine
- Severe fatigue or weakness
- Pain in the upper right abdomen
- Nausea or vomiting that won’t go away
If you notice any of these, stop taking isoniazid and call your doctor immediately. Liver failure from isoniazid is rare-but it can be fatal if ignored.
Another rare but serious side effect is peripheral neuropathy, which causes numbness, tingling, or burning in the hands and feet. This happens because isoniazid lowers vitamin B6 (pyridoxine) levels. That’s why doctors often prescribe a daily B6 supplement along with isoniazid, especially for people at higher risk: diabetics, people with HIV, alcohol use disorder, or kidney disease.
Less common side effects include mood changes, seizures, or even psychosis. These are extremely rare but should be taken seriously. If you feel unusually anxious, depressed, or hear voices, tell your doctor right away.

How long do you take isoniazid-and why timing matters
For latent TB, the standard course is 6 months. In some cases, doctors may prescribe 9 months for better protection, especially in children or people with HIV. For active TB, isoniazid is always part of a 4-drug combo for the first 2 months, then continued for at least 4 more months (total 6 months minimum).
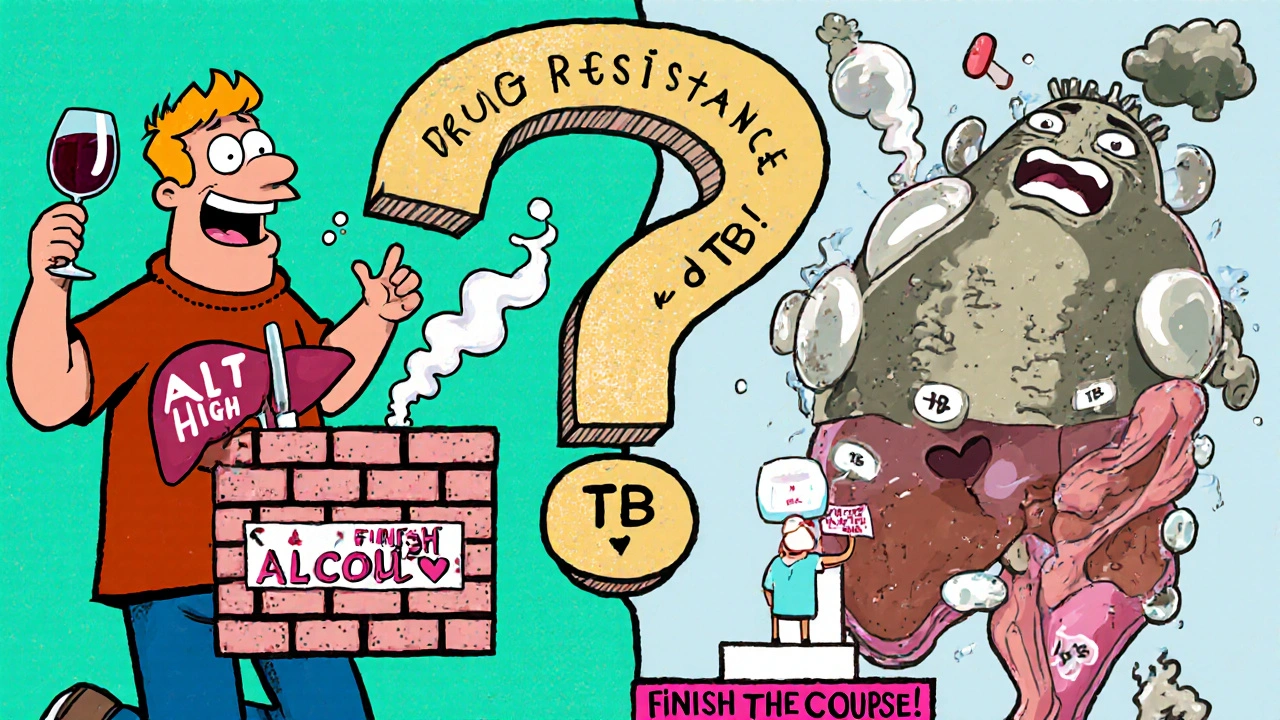
Why not stop when you feel better? Because TB bacteria are sneaky. They can go dormant in hard-to-reach areas of the lungs. If you stop early, the strongest bacteria survive and come back-this time resistant to the drug. Drug-resistant TB is harder to treat, takes longer, costs more, and can spread to others.
Directly Observed Therapy (DOT) is used in many parts of the UK to make sure people take every dose. A nurse or community worker watches you swallow the pill. It sounds strict, but it’s one of the most effective ways to prevent drug resistance. Studies show DOT improves completion rates from 60% to over 90%.
What to avoid while taking isoniazid
There are a few things you should absolutely avoid while on isoniazid:
- Alcohol-Drinking while on isoniazid increases liver damage risk by up to 5 times. Even moderate drinking (like a glass of wine a night) isn’t safe during treatment.
- Tyramine-rich foods-While not as strict as with older antidepressants, foods like aged cheese, cured meats, soy sauce, and tap beer can cause dangerous spikes in blood pressure in rare cases. It’s not common, but if you’re unsure, ask your pharmacist.
- Other liver-toxic drugs-Avoid acetaminophen (paracetamol) in high doses. Don’t take herbal supplements like kava or green tea extract without checking with your doctor. Many over-the-counter painkillers and cold medicines can stress your liver too.
Also, don’t skip your blood tests. Liver function tests (ALT, AST, bilirubin) are simple, quick, and essential. Most clinics do them at the start, then again at 2 and 4 weeks. After that, every 4-8 weeks if you’re on long-term treatment.
What happens if you miss a dose?
If you miss one dose, take it as soon as you remember-if it’s within a few hours. If it’s almost time for your next dose, skip the missed one and go back to your regular schedule. Never double up.
Missing a few doses isn’t a disaster, but it increases your chance of drug resistance. If you miss more than 10% of your doses over a month, your doctor may switch you to a different regimen or add another drug. Some people use pill boxes or phone alarms to stay on track. Apps like MyTB Tracker are used in NHS clinics to help patients remember doses.
Is isoniazid safe during pregnancy or breastfeeding?
Yes-but with caution. The NHS and WHO both recommend isoniazid for pregnant women with active or latent TB. Untreated TB poses a far greater risk to mother and baby than the drug. Isoniazid crosses the placenta, but studies show no increased risk of birth defects.
For breastfeeding mothers, isoniazid passes into breast milk in small amounts. The amount is not enough to harm the baby. In fact, the baby is often given a low dose of isoniazid as a preventive measure if the mother has active TB. Vitamin B6 is still recommended for the mother to prevent nerve damage.
Alternatives to isoniazid
If you can’t take isoniazid due to liver issues, allergies, or drug resistance, there are other options:
- Rifampin-Used alone for 4 months for latent TB. Less liver risk than isoniazid, but can turn body fluids orange.
- Rifapentine-Taken once a week with directly observed therapy. A 3-month course replaces the 9-month isoniazid plan for some people.
- Levofloxacin or moxifloxacin-Fluoroquinolones used in drug-resistant TB cases or when first-line drugs aren’t an option.
Each alternative has its own side effects and costs. Rifampin can interfere with birth control pills and blood thinners. Levofloxacin may cause tendon damage. Your doctor will choose based on your health history, not just convenience.
Final thoughts: Isoniazid isn’t just a pill-it’s a lifeline
Isoniazid is old, but it’s not outdated. It’s still the most cost-effective, proven tool we have to stop TB before it kills. In Scotland, TB rates are low but not gone. Every year, around 300 cases are reported, mostly in cities like Glasgow and Edinburgh. Many of these are in people born abroad or living in crowded housing.
Taking isoniazid isn’t glamorous. It’s daily pills for months, blood tests, avoiding wine, and remembering to call your clinic. But it’s one of the few medical treatments that can stop a disease from spreading to your family, your coworkers, your community.
If you’ve been told to take isoniazid, don’t ignore it. Talk to your doctor if you’re scared of side effects. Ask about B6 supplements. Use a pill reminder. Get your liver tests done. This drug saved your life-or could. Don’t let fear stop you from finishing what you started.
Can isoniazid cause permanent liver damage?
Permanent liver damage from isoniazid is rare, occurring in less than 1% of people. Most cases are caught early through blood tests and reverse when the drug is stopped. But if liver injury is ignored and treatment continues, it can lead to acute liver failure, which may require a transplant. That’s why regular liver monitoring is critical-especially after the first month of treatment.
Is isoniazid still used in the UK today?
Yes. Isoniazid remains a first-line drug for both latent and active tuberculosis in the UK. The NHS follows WHO and Public Health England guidelines that still list isoniazid as the gold standard for prevention and treatment. Newer drugs are used when resistance is suspected or when patients can’t tolerate isoniazid, but it’s still the most prescribed TB medication in the country.
Why do I need to take vitamin B6 with isoniazid?
Isoniazid interferes with how your body uses vitamin B6 (pyridoxine), which is essential for nerve function. Without enough B6, you can develop peripheral neuropathy-numbness, tingling, or pain in your hands and feet. Taking a daily 10-25 mg B6 supplement prevents this side effect. It’s especially important for people who are malnourished, diabetic, pregnant, or drink alcohol regularly.
Can I drink alcohol while taking isoniazid?
No. Alcohol increases the risk of liver damage from isoniazid by up to five times. Even small amounts-like one glass of wine or beer a day-can be dangerous. Doctors strongly advise complete abstinence from alcohol during treatment and for at least one month after stopping. This isn’t a suggestion-it’s a safety rule.
How do I know if isoniazid is working?
For latent TB, you won’t feel any different-because the bacteria aren’t causing symptoms. The goal is prevention, not relief. For active TB, you should start feeling better within 2-4 weeks: less coughing, less fever, more energy. But feeling better doesn’t mean the bacteria are gone. You must finish the full course, even if you feel fine. The only way to confirm it’s working is through follow-up tests like chest X-rays and sputum cultures.
What happens if I stop isoniazid early?
Stopping early increases your risk of relapse-and drug-resistant TB. TB bacteria that survive incomplete treatment can mutate and become resistant to isoniazid and other drugs. This leads to multidrug-resistant TB (MDR-TB), which requires 18-24 months of treatment with more toxic, expensive drugs. In some cases, it’s untreatable. Completing your course isn’t optional-it’s the only way to protect yourself and others.