Getting your medicine on time, every time, sounds simple. But for nearly half of people with chronic conditions, it’s not. The World Health Organization says about 50% of patients don’t take their meds as prescribed. That’s not laziness. It’s forgetfulness, side effects, cost, fear, or just feeling alone in the struggle. That’s where medication compliance support groups and community programs step in-not to lecture, but to walk beside you.
Why Medication Adherence Isn’t Just About Memory
People think if you just remind someone to take their pills, they’ll do it. But studies show that handing out a flyer or a pill organizer only moves the needle a little. The real game-changer? Connection. When someone who’s been there-someone who knows what it’s like to feel dizzy from blood pressure meds or to skip insulin because the cost hurt too much-shares their story, something shifts. You stop feeling broken. You start feeling understood. A 2020 review in the Journal of Medical Care found peer-led support groups had more than double the impact of educational materials alone. The effect size? Cohen’s d=0.40. That’s not a tiny win. That’s the kind of change that lowers hospital readmissions by 15 to 30% for people with diabetes, heart disease, or depression.How These Programs Actually Work
Not all support programs are the same. There are three main types you’ll find:- Hospital-based peer groups: Meet once or twice a week in a clinic room. Usually 8 to 12 people. Led by someone who’s been managing their own condition for at least two years. No doctors in the room-just real talk about side effects, insurance headaches, and how to remember pills when you’re traveling.
- Community health worker visits: A trained local worker comes to your home, usually 4 to 12 times over a few months. They don’t give medical advice. They ask: “What’s making it hard?” Then they help you find solutions-like connecting you to a pharmacy that offers discounts, or setting up a phone alarm with your grandkid’s voice saying, “Time for your med.”
- Digital peer platforms: Apps and online forums where people share tips 24/7. Think Reddit threads or PatientsLikeMe. You can post at 2 a.m. when you’re scared your heart is racing. Someone responds within minutes: “I felt that too. Here’s what worked for me.”
Family Support Makes a Bigger Difference Than You Think
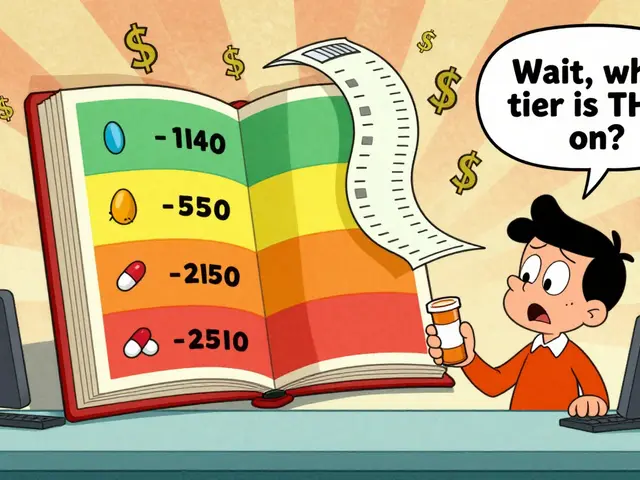
It’s not just peers. Family involvement is one of the strongest predictors of adherence. A 2021 study reviewed 14 studies and found 11 showed clear links between family support and better pill-taking. Not because they nagged. Because they showed up. One woman in North Carolina told researchers her husband started putting her diabetes meds in his wallet every morning. “He doesn’t say anything. He just holds out his hand when we leave the house. I take mine. He takes his.” That’s not a program. That’s love in action. Programs that train family members to be part of the support team see better long-term results than those that focus only on the patient. A 2023 study in Frontiers in Pharmacology found face-to-face peer groups had 28% higher long-term adherence than apps alone-because apps can’t hug you when you cry over a $400 co-pay.
The Hidden Barriers: Rural, Language, and Culture
These programs work-but not for everyone. In rural areas, participation drops by 32% because there’s no group nearby, and driving 50 miles to a meeting isn’t realistic when you’re on oxygen. Language matters too. Only 22% of U.S. programs offer support in languages other than English-even though 25% of the population has limited English skills. A 2022 study in BMC Health Services Research found African American participants in hypertension groups were 35% more likely to stick with the program when the facilitator shared their cultural background. Same language. Same experiences. Same trust. And then there’s the cost. Nonprofit programs often run on grants of $75,000 to $150,000 a year. When those run out, the group shuts down. That’s why 41% of nonprofit programs reported financial instability in 2023. No one talks about this-but it’s why so many people get excited about a program… then it disappears.What Makes a Program Actually Work?
Not all groups are created equal. The difference between one that helps and one that doesn’t? Training. Programs with facilitators who’ve had at least 40 hours of training see 37% better adherence than those with less. Why? Because good facilitators don’t give advice. They listen. They ask: “What’s stopping you?” Not “Why didn’t you take it?” Effective programs also combine strategies. The Agency for Healthcare Research and Quality found programs using four or more behavior-change techniques-like reminders, problem-solving, social support, and simplifying regimens-were 31% more effective than single-method ones. And here’s something surprising: pharmacists are the secret weapon. A Cochrane Review found pharmacist-led groups improved adherence by 23% more than doctor-led ones. Why? They know your meds inside out. They can tell you why your blood pressure pill makes you cough, or how to split a pill safely. They’re not just handing out bottles. They’re problem-solvers.Real Stories: What People Are Saying
On Reddit, a user named DiabetesWarrior87 wrote: “I was missing 3 to 4 doses a week. My A1c was 8.5%. After six months in a weekly support group, I was missing less than one. My A1c dropped to 6.9%.” A 2022 survey of 12,450 users on PatientsLikeMe found 78% improved their adherence because of group support. The top reason? “Hearing how others manage side effects.” Not the doctor’s pamphlet. Not the app notification. The real talk. But it’s not perfect. Forty-two percent of participants in a NAMI survey said scheduling conflicts made it hard to keep going. Twenty-nine percent felt uncomfortable in group settings. And 27% complained about lack of medical oversight-like when someone says, “Just take your pills,” but doesn’t know your meds interact badly with your thyroid drug.
What’s New in 2025?
The field is evolving. In 2023, Medicare launched a $50 million program to hire community health workers to help dual-eligible patients (those on Medicare and Medicaid) with their meds. The FDA approved the first digital therapeutic for medication adherence-reSET-O-which pairs an app with live peer coaching. The biggest breakthrough? Hybrid models. A 2023 study found combining weekly in-person peer meetings with daily text reminders boosted adherence by 34% in hypertension patients. That’s the future: human connection, backed by tech.What You Can Do Right Now
If you’re struggling with meds:- Ask your pharmacist: “Do you have a support group or patient navigator?”
- Check with your local hospital or community center. Many run free groups you didn’t know about.
- Try a moderated online forum like PatientsLikeMe or HealthUnlocked. You don’t have to speak. Just read. Often, that’s enough to start feeling less alone.
- If you’re a family member: Don’t nag. Ask, “What’s the hardest part?” Then sit with them while they figure it out.
- Train your facilitators-40 hours minimum.
- Include pharmacists. They’re not just dispensers. They’re adherence experts.
- Offer sessions in multiple languages.
- Use the Morisky scale to track progress. Most programs still don’t. That’s like flying blind.
Final Thought: It’s Not About Willpower
Medication compliance isn’t about being disciplined. It’s about being supported. You don’t need more reminders. You need someone who knows what it’s like to sit on the edge of your bed, holding two pills, wondering if it’s worth it. That’s what these programs give you: not a cure. Not a magic fix. But the quiet certainty that you’re not alone. And sometimes, that’s all it takes to keep going.Do support groups really help people take their meds?
Yes. Studies show peer-led support groups improve medication adherence by 15-30% compared to no support. People who attend regularly are more likely to stick to their regimen because they feel understood, get practical tips, and have accountability from others who’ve been there.
Are these programs free?
Many community-based programs are free, funded by grants or nonprofits. Hospital-based programs may be covered by insurance or included as part of care. Digital platforms often have free tiers. Some programs charge small fees, but financial aid is usually available if needed.
Can I join if I live in a rural area?
Yes, but options may be limited. Rural areas have 47% fewer programs per capita than cities. Look for virtual groups, phone-based support, or mobile health workers who travel to your area. Some programs offer mailed pill organizers with check-in calls.
What if I’m uncomfortable talking in a group?
You don’t have to speak. Many people listen for months before sharing. Online forums offer anonymity. One-on-one visits with a community health worker are also an option. The goal is support-not performance.
How long do I need to attend to see results?
Most people notice improvements in 2 to 3 months. Long-term adherence (over 6 months) is strongest when participation continues. Dropout rates are around 22% by 6 months, so consistency matters. Programs with text reminders or family involvement see lower dropouts.
Can family members join these groups?
Many programs welcome family members. In fact, studies show involvement from spouses, children, or caregivers improves adherence significantly. Some groups even have separate sessions for families to learn how to help without nagging.
Do these programs work for mental health meds?
Yes. For depression, bipolar disorder, and schizophrenia, peer support is especially powerful. People often stop meds because they feel stigmatized or misunderstood. Support groups provide safety, reduce isolation, and normalize the experience-leading to better adherence than standard counseling alone.
What if my meds are too expensive?
Many programs connect participants with patient assistance programs, coupons, or generic alternatives. Pharmacists in these groups often help navigate savings options. Some nonprofits even provide free medication for qualifying individuals. Don’t skip pills because of cost-ask for help.
How do I find a program near me?
Start with your pharmacist, local hospital, or community health center. Search online for “[your condition] support group near me.” Organizations like the American Heart Association, American Diabetes Association, and NAMI often list local chapters. Medicare Advantage plans may also offer referrals.
Are digital apps as good as in-person groups?
Apps help with reminders and tracking, but they don’t replace human connection. Studies show face-to-face peer groups lead to 28% higher long-term adherence because of emotional support. The best option? Hybrid: use an app for reminders and join a group for motivation and shared experience.