Clinically Isolated Syndrome is a single neurological episode caused by inflammation or demyelination in the central nervous system, often the first hint of multiple sclerosis. Approximately 30% of people with CIS develop full‑blown multiple sclerosis (MS) within five years, especially when MRI shows active lesions. Early pharmacological intervention can dramatically lower that risk, turning a potentially progressive disease into a manageable condition.
- Identify the key medication classes used in CIS.
- Understand how MRI findings guide treatment choice.
- Compare efficacy and safety of first‑line and high‑efficacy disease‑modifying therapies (DMTs).
- Learn when to involve a neurologist and what monitoring looks like.
- Know the common side‑effects and how to mitigate them.
Why Medication Matters After a CIS Event
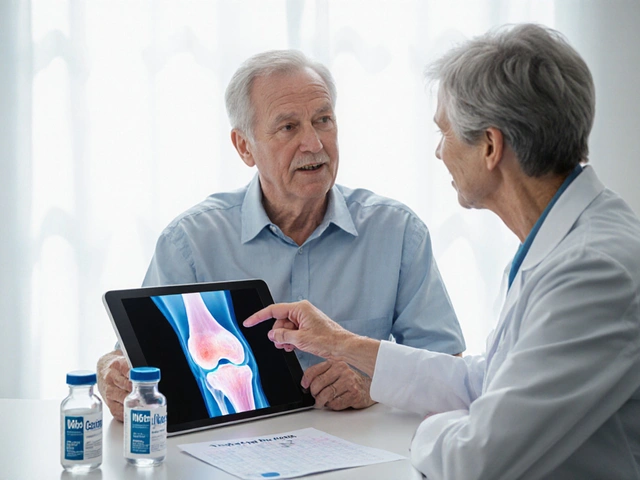
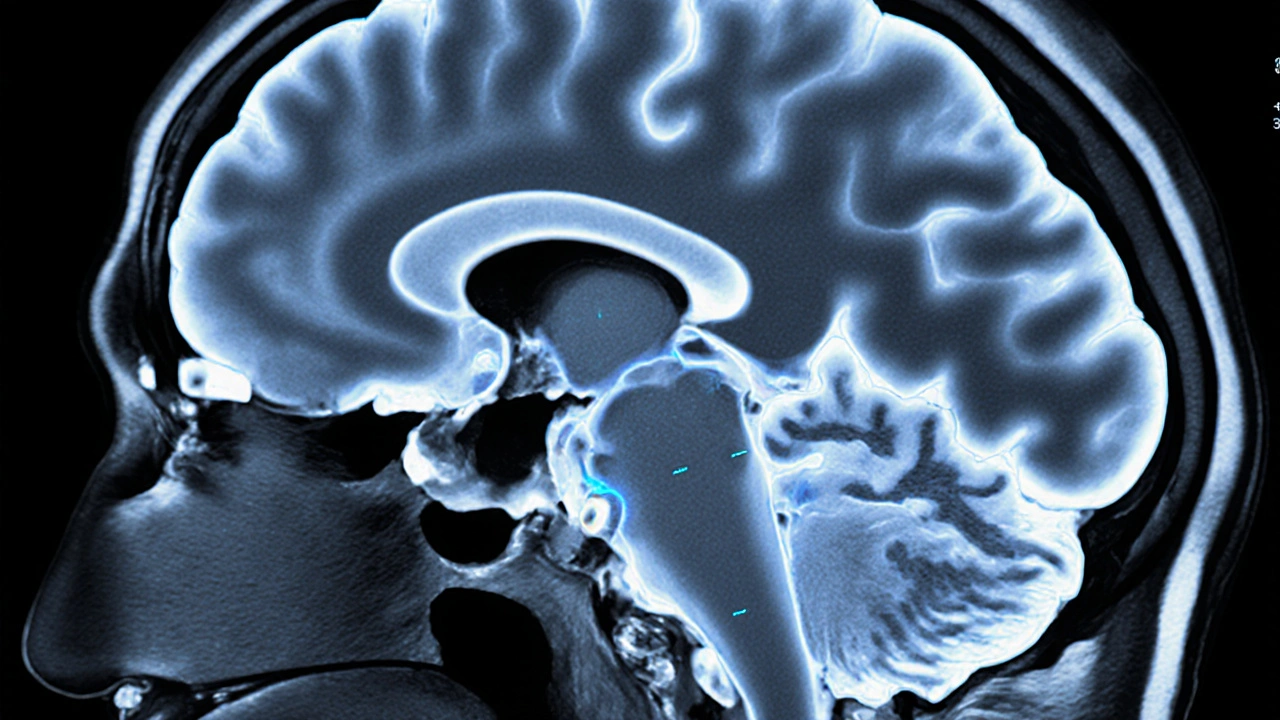
When a clinician labels an episode as CIS, the main question is: will the immune system keep attacking my nervous system? The answer lies in two pieces of data - the MRI scan and the presence of oligoclonal bands in cerebrospinal fluid. A high lesion load or gadolinium‑enhancing lesions increase conversion risk to MS. Medications classified as Disease‑Modifying Therapies (DMTs) work by dampening the immune response, thereby reducing new lesion formation and clinical relapses.
First‑Line DMTs: Interferon Beta and Glatiramer Acetate
Historically, the two workhorses for early CIS treatment are Interferon beta and Glatiramer acetate. Both have decades of safety data and are administered via injection.
- Interferon beta reduces annualized relapse rate (ARR) by roughly 30% and slows brain‑volume loss.
- Common side‑effects include flu‑like symptoms, injection site redness, and transient liver enzyme elevation.
- Glatiramer acetate mimics myelin basic protein, diverting the immune attack; it lowers ARR by 25‑35% with fewer systemic flu‑like reactions.
- Injection site reactions are the most frequent complaint, but most patients find them tolerable after the first few weeks.
Choosing between them often depends on lifestyle (weekly vs. daily injections) and personal tolerance for flu‑like side‑effects.
High‑Efficacy Oral and Infusion Options
When MRI shows multiple active lesions or the patient has a high risk profile, clinicians may step up to higher‑potency agents.
| Medication | Route | Key Efficacy Metric (ARR reduction) | Major Safety Concern |
|---|---|---|---|
| Interferon beta | Injection (weekly or three‑times weekly) | ~30% | Flu‑like symptoms, liver enzymes |
| Glatiramer acetate | d>Injection (daily) | ~25‑35% | Injection site reactions |
| Fingolimod | Oral (once daily) | ~45% | Cardiac conduction delay, infections |
| Ocrelizumab | IV infusion (every 6 months) | ~55% | Infusion reactions, rare malignancy risk |
Oral fingolimod offers the convenience of a pill but requires cardiac monitoring at start‑up because it can pause the heart’s pacemaker activity. Ocrelizumab, a monoclonal antibody targeting CD20‑positive B cells, delivers the strongest ARR reduction but comes with infusion‑related reactions and a need for pre‑treatment screening for hepatitis B.
How a Neurologist Personalizes the Treatment Plan
In the UK, referral to a Neurologist is standard after a CIS diagnosis. The specialist reviews:
- Baseline MRI - number, size, and enhancement of lesions.
- CSF analysis - presence of oligoclonal bands.
- Patient age, gender, and family history of MS.
- Vaccination status and comorbidities (e.g., liver disease, cardiac issues).
Using that data, the neurologist may apply the McDonald criteria to determine whether the patient already meets MS diagnostic thresholds. If not, the neurologist will often start a low‑risk DMT while scheduling repeat MRI at 6‑12 months.
Monitoring Treatment Effectiveness
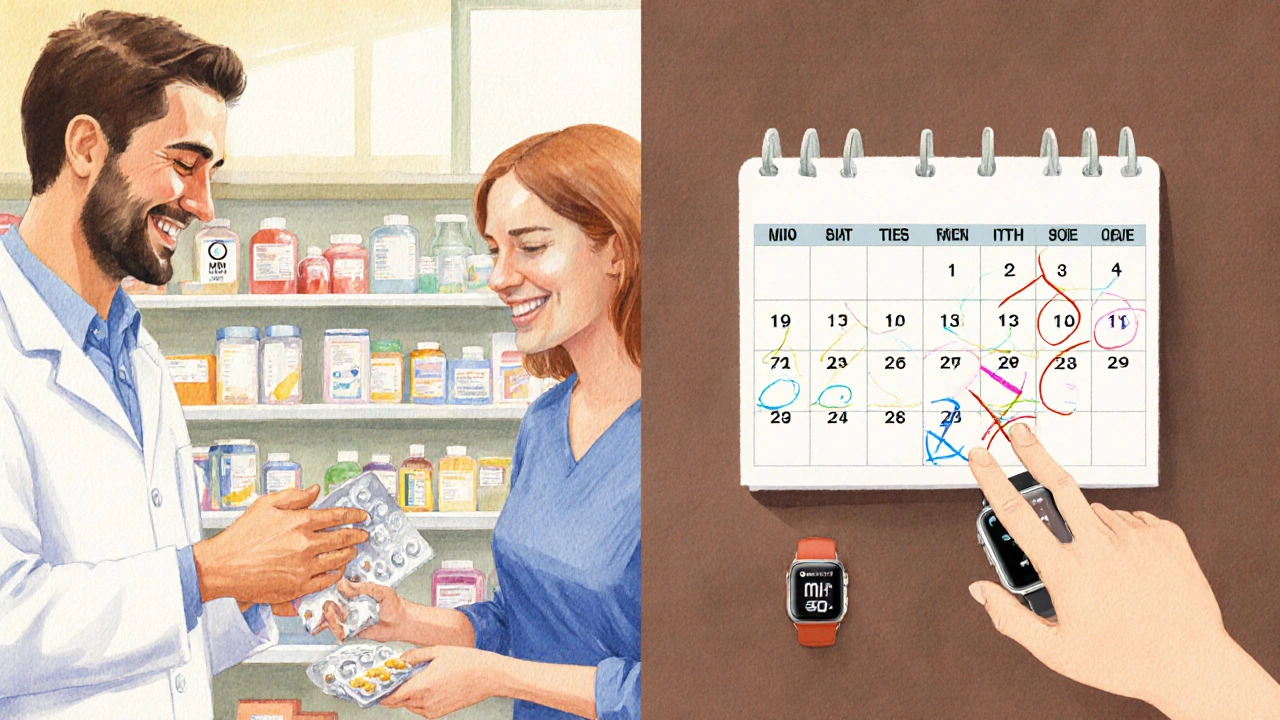
Even after therapy begins, vigilance remains crucial. The typical monitoring schedule looks like:
- Clinical review every 3-6 months for relapse signs or new neurological deficits.
- Blood work before each dosing cycle for liver function, lymphocyte count, and infection markers.
- Follow‑up MRI at 12 months, then every 1-2 years, to compare new versus old lesions.
If serial MRIs reveal no new lesions and the patient is relapse‑free, the neurologist may continue the current DMT. Conversely, evidence of breakthrough disease prompts a switch to a higher‑efficacy agent.
Managing Common Side‑Effects
Side‑effects are often the reason patients stop therapy prematurely. Practical tips include:
- For interferon‑induced flu‑like symptoms, take the injection after bedtime and use acetaminophen in the morning.
- Injection site pain from glatiramer can be eased with topical lidocaine or rotating injection sites.
- Fingolimod‑related hypertension is monitored with regular blood pressure checks; dose adjustment may be needed.
- Ocrelizumab infusion reactions are mitigated with pre‑medication (steroid, antihistamine) and a 30‑minute observation period.
Open communication with the neurologist helps tailor these strategies to each individual’s tolerance.
Future Directions: Emerging Therapies and Biomarkers
Research published by leading neurologic societies in 2023 highlighted two promising avenues:
- Siponimod, a next‑generation sphingosine‑1‑phosphate receptor modulator, shows comparable efficacy to ocrelizumab with a more convenient oral regimen.
- Neurofilament light chain (NfL) levels in serum are emerging as a quantitative biomarker for subclinical disease activity, potentially allowing earlier treatment switches.
While still awaiting regulatory approval for CIS, these tools hint at a future where medication decisions are guided by real‑time biology rather than just MRI snapshots.
Putting It All Together: A Decision Flow for Patients
Below is a simplified flow that captures the typical journey from CIS diagnosis to long‑term management:
- Diagnose CIS → Obtain baseline MRI and CSF.
- Risk stratify: high lesion load or oligoclonal bands = high risk.
- Start first‑line DMT (interferon beta or glatiramer) if low‑risk; consider high‑efficacy DMT (fingolimod, ocrelizumab) if high‑risk.
- Monitor clinically and radiologically every 6-12 months.
- If new lesions or relapse → escalates to higher‑efficacy agent or switches class.
- Re‑assess biomarkers (e.g., NfL) when available to fine‑tune therapy.
This roadmap underscores why Clinically Isolated Syndrome medication is not a one‑size‑fits‑all proposition; it evolves with the patient’s disease trajectory.
Frequently Asked Questions
Can I delay treatment after a CIS event?
Delaying treatment is generally discouraged if MRI shows active lesions. Early DMT can cut the conversion risk to MS by about half. A few low‑risk patients may opt for watchful waiting, but they need strict MRI surveillance.
Do oral DMTs work as well as injectables?
Yes, oral agents like fingolimod and siponimod have demonstrated comparable or even superior ARR reductions to interferon beta, though they carry distinct safety profiles that require monitoring.
What is the role of MRI in treatment choice?
MRI quantifies lesion number, size, and activity. A high lesion count or gadolinium‑enhancing lesions push clinicians toward high‑efficacy DMTs. Conversely, a clean MRI may justify starting with a low‑risk injectable.
Are there lifestyle changes that boost medication effectiveness?
Maintaining a balanced diet, regular low‑impact exercise, adequate sleep, and avoiding smoking can reduce overall inflammation and may improve DMT outcomes. Vaccinations (flu, COVID‑19) are also recommended before starting immunosuppressive drugs.
What should I do if I experience a relapse while on medication?
Contact your neurologist immediately. Early steroid treatment (e.g., high‑dose methylprednisolone) can speed recovery. The neurologist will reassess MRI and may consider switching to a more potent DMT.