Hidradenitis suppurativa isn't just a rash. It’s a chronic, painful condition that turns hair follicles into deep, recurring abscesses that leak, scar, and cripple daily life. Think of it as your body’s immune system going haywire inside the sweat glands - usually in the armpits, groin, or under the breasts. These aren’t pimples you can pop. They’re hard, fist-sized nodules that burn, ooze, and often connect under the skin through tunnels called sinus tracts. For many, it starts in their 20s, hits hardest in women, and gets worse with weight gain, smoking, or stress. Until recently, the only real options were antibiotics that stopped working, hormonal pills with side effects, or surgery that left scars and didn’t stop the cycle.
Why Do These Nodules Form?
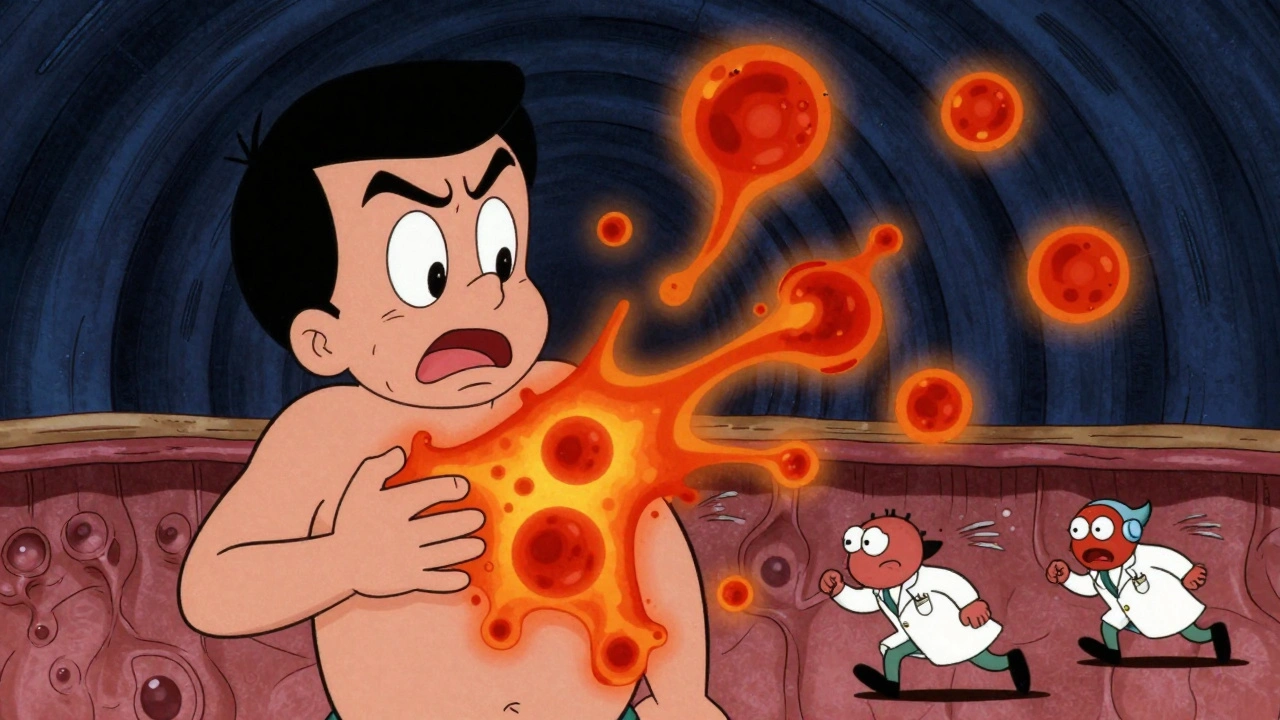
The root cause isn’t dirt or poor hygiene. It starts when dead skin cells and oils clog a hair follicle. That blockage triggers inflammation deep in the tissue, and the body’s immune system goes into overdrive. Key players like TNF-alpha, IL-17, and IL-23 flood the area, turning a small bump into a swollen, pus-filled abscess. Over time, these abscesses don’t heal properly. Instead, they tunnel under the skin, forming networks that keep re-infecting. That’s why HS gets worse over years - it’s not just surface-level. It’s a systemic inflammatory disease that affects more than your skin.
Biologic Therapy: A Game-Changer
Before 2015, there was no FDA-approved drug specifically for HS. Then came adalimumab (Humira), the first biologic approved to treat moderate-to-severe cases. Biologics are different from regular pills. They’re made from living cells and target one specific part of the immune system. Instead of suppressing your whole immune response, they silence just the signals causing the inflammation. This precision means fewer side effects than old-school immunosuppressants.
Today, three biologics are approved for HS in the U.S., each with a different target:
- Adalimumab blocks TNF-alpha, the main inflammatory signal. Given as a weekly or every-other-week injection, it helps about 42% of patients see at least half their lesions clear by week 12.
- Secukinumab targets IL-17A. Approved in early 2024, it works faster for many - 45% of users hit the 50% improvement mark by week 16.
- Bimekizumab is the newest and most powerful. It blocks both IL-17A and IL-17F, two closely linked signals. In clinical trials, 67% of patients saw half their lesions disappear by week 16 - the highest response rate ever recorded for HS.
These aren’t magic cures. But for people who’ve suffered for years, they’re life-changing. One woman in Edinburgh described it like this: “After 12 years of constant pain, I could finally wear a t-shirt without hiding. The burning stopped. The draining stopped. I slept through the night.”
How Do They Compare?
Not all biologics are the same. Here’s how they stack up based on real data:
| Biologic | Target | Dosing | HiSCR50 at Week 12-16 | Common Side Effects |
|---|---|---|---|---|
| Adalimumab (Humira) | TNF-alpha | 40 mg weekly or every other week | 41.8% | Injection site reactions, upper respiratory infections |
| Secukinumab (Cosentyx) | IL-17A | 300 mg weekly x5, then every 4 weeks | 44.5% | Headache, fungal infections, mild diarrhea |
| Bimekizumab (Bimzelx) | IL-17A and IL-17F | 320 mg every 4 weeks (after loading dose) | 66.9% | Candida infections, fatigue, headache |
Adalimumab has been around the longest and works well, especially for people with deep scarring. But if your main problem is new, painful abscesses, secukinumab or bimekizumab may work faster and better. Bimekizumab’s dual action gives it the edge in clinical numbers - but it’s also the most expensive. Monthly costs in the U.S. range from $5,800 to $6,900. Insurance often requires trying other treatments first, and even then, approvals can take months.

Who Benefits Most?
Biologics aren’t for everyone. They’re recommended for Hurley Stage II or III HS - meaning you have multiple abscesses and tunnels under the skin. If you only get occasional bumps, antibiotics or lifestyle changes might be enough. But if you’ve had this for years, and it’s spreading, biologics are your best shot at real relief.
Experts agree: early treatment stops damage. Once scarring and sinus tracts form, they’re permanent. Surgery can remove them, but the disease often comes back. Biologics can stop the process before it gets that far. One dermatologist in Glasgow told me: “I’ve seen patients who waited five years to start treatment. Their skin was a map of scars. No drug could fix that. But if they’d started sooner, they might have avoided most of it.”
What to Expect When You Start
Starting a biologic isn’t like popping a pill. You’ll need screening first: a TB test, hepatitis check, and a review of your heart health. These drugs lower your body’s ability to fight certain infections, so you can’t start if you’re already sick with something serious.
After your first injection, you won’t feel better overnight. Most people notice less pain and fewer new abscesses after 4 to 8 weeks. Full results take 12 to 16 weeks. Your doctor will track your progress using the IHS4 score - a simple way to count active lesions, abscesses, and nodules. If you haven’t improved by week 12, you may switch to another biologic.
Side effects are usually mild: redness at the injection site, headaches, or a cold. But serious infections like tuberculosis or fungal infections can happen. That’s why you need regular check-ins. Some patients also see their cholesterol improve - triglycerides drop, HDL rises - suggesting these drugs help your whole body, not just your skin.
Real Patient Experiences
Online communities like MyHSteam and Reddit’s r/hidradenitis are full of stories. One man in Scotland switched from adalimumab to bimekizumab after a year with no improvement. Within six weeks, his groin abscesses vanished. “I went from needing painkillers daily to walking without flinching,” he wrote.
But it’s not all smooth. Cost is a huge barrier. Even with insurance, some pay $1,200 a month out of pocket. Others get denied coverage entirely. A 2023 survey found 33% of users quit biologics because of cost. Medicaid patients are approved at less than half the rate of those with private insurance.
Many also report needing to combine biologics with lifestyle changes. Quitting smoking cuts flare-ups by 60%. Losing even 10% of body weight improves response rates. One woman in Edinburgh lost 35 pounds and started walking daily. “The biologic helped, but my body finally stopped fighting itself,” she said.
What’s Next?
The future is bright. Three new biologics are in late-stage trials:
- Guselkumab blocks IL-23 - a signal upstream of IL-17. Early results show 58% improvement.
- Spesolimab targets IL-36, which may help with skin inflammation in ways we didn’t understand before.
- TAK-279 works inside immune cells to block a key enzyme, TYK2, and looks promising in early data.
Researchers are even testing combinations - like using bimekizumab with minor surgery to remove tunnels. One study showed 89% of patients cleared their lesions with this combo, compared to 67% with the drug alone.
Scientists are also looking for biomarkers - blood tests or gene patterns - that can predict who will respond to which drug. A 2024 study found a 12-gene signature that predicted adalimumab success with 85% accuracy. That could mean less trial and error in the future.
Bottom Line
Hidradenitis suppurativa doesn’t have to be a life sentence. Biologic therapy has changed everything for those with moderate-to-severe cases. You don’t have to live with constant pain, embarrassment, or isolation. The right drug can bring back normalcy - sleeping through the night, wearing what you want, being active without fear.
But timing matters. The earlier you start, the less damage you’ll have. And it’s not just about the drug - it’s about working with your doctor, managing your weight, quitting smoking, and sticking with treatment. It’s not easy. But for the first time, there’s real hope.
If you’ve been told “it’s just a skin thing” - don’t believe it. HS is serious. And now, there’s a powerful way to fight it.