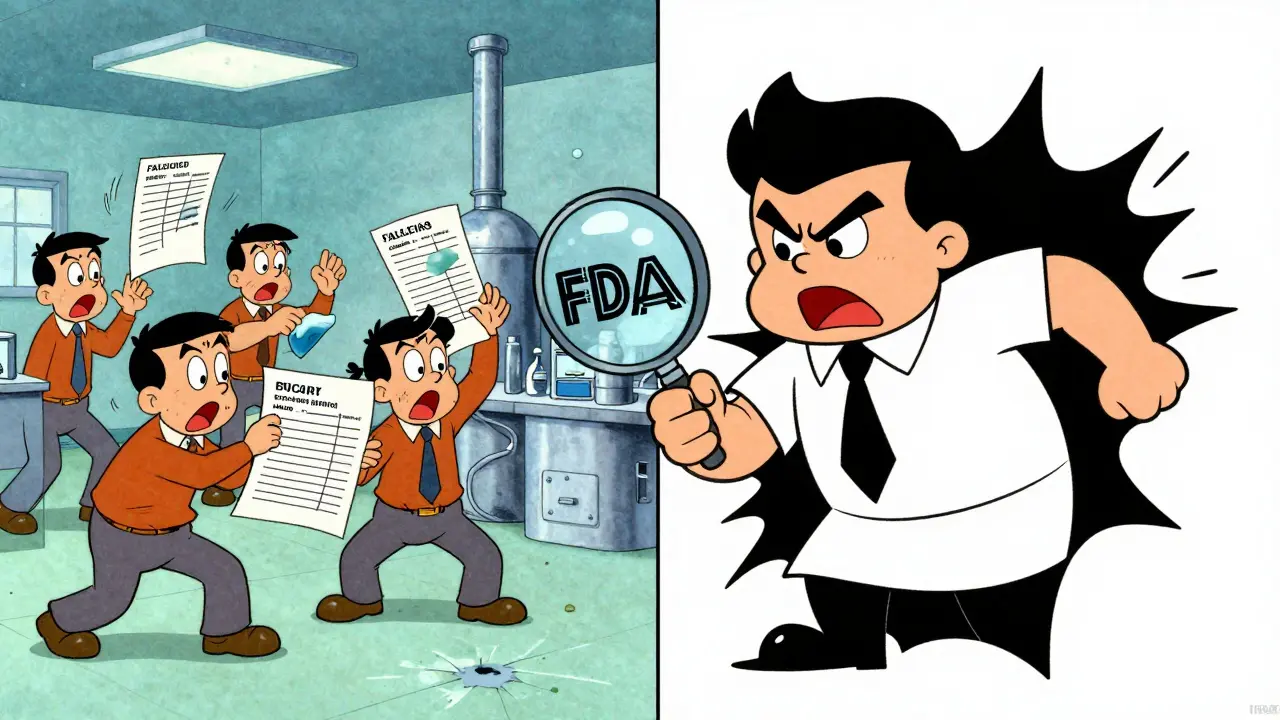
More than 90% of the generic drugs Americans take every day are made overseas. Most come from factories in India and China. But here’s the problem: the U.S. Food and Drug Administration (FDA) used to inspect these foreign plants with weeks of notice. That meant companies had time to clean up, fix records, and hide problems. In 2024, nearly half of all foreign inspections found serious issues-data falsification, contamination, and broken quality controls. Domestic plants? Only about 20% had the same problems. And they were inspected without warning.
Why Foreign Factories Got a Different Standard
For decades, the FDA treated foreign and domestic drug makers differently. Domestic facilities faced surprise inspections. Foreign ones got letters saying, “We’ll be there in 8 weeks.” That gave manufacturers time to train staff, fix equipment, and even rewrite lab logs. It wasn’t illegal-but it wasn’t fair. And it wasn’t safe. The numbers don’t lie. In 2024, foreign facilities had a 38.7% failure rate for data integrity violations. Domestic facilities? Just 17.2%. Contamination control problems showed up in 22.4% of foreign inspections. At home? Only 9.8%. The FDA had inspectors, but not enough to cover over 90 countries. They did about 3,000 foreign inspections a year compared to 12,000 domestic ones. With 80% of active drug ingredients and 40% of finished pills coming from abroad, that gap was a public health risk.What Changed in 2025
On May 6, 2025, everything shifted. FDA Commissioner Marty Makary announced a new policy: unannounced inspections for foreign manufacturers would jump from 15% to at least 50% by mid-2026. That means a plant in Hyderabad or Shanghai could get a visit with less than 48 hours’ notice. No warning. No time to hide. This wasn’t just a policy tweak. It was a response to pressure. In April 2025, Senators Kirsten Gillibrand and Tim Scott demanded answers after ProPublica uncovered cases where the FDA allowed drugs from banned facilities to enter the U.S. market. One Indian company, Sun Pharma, had its plant shut down in 2021 for falsifying data-yet four of its drugs were still approved for sale in America months later. That kind of inconsistency eroded trust. President Trump’s Executive Order 14135, signed the day before Makary’s announcement, forced the FDA to eliminate the inspection gap within 18 months. The agency responded by hiring 200 new international inspectors and doubling its inspection budget for foreign sites. They’re also working with regulators in the EU, Japan, and Australia to share inspection data and avoid duplicate checks.CGMP: The Rules Everyone Must Follow
Whether you’re making pills in Ohio or Odisha, you must follow Current Good Manufacturing Practices (CGMP). These aren’t suggestions. They’re federal law. CGMP covers everything: how staff are trained, how equipment is cleaned, how raw materials are tested, and how final products are stored. FDA inspectors show up with Form 483. It’s not a report card. It’s a list of violations. Common findings? Missing batch records, uncalibrated machines, mold in clean rooms, or lab results that don’t match what’s written down. One foreign manufacturer got cited for using the same water filter for three years-long past its expiration date. Another had employees manually changing test results because automated systems flagged failures too often. The rules are the same. But enforcement wasn’t. Now, it’s catching up.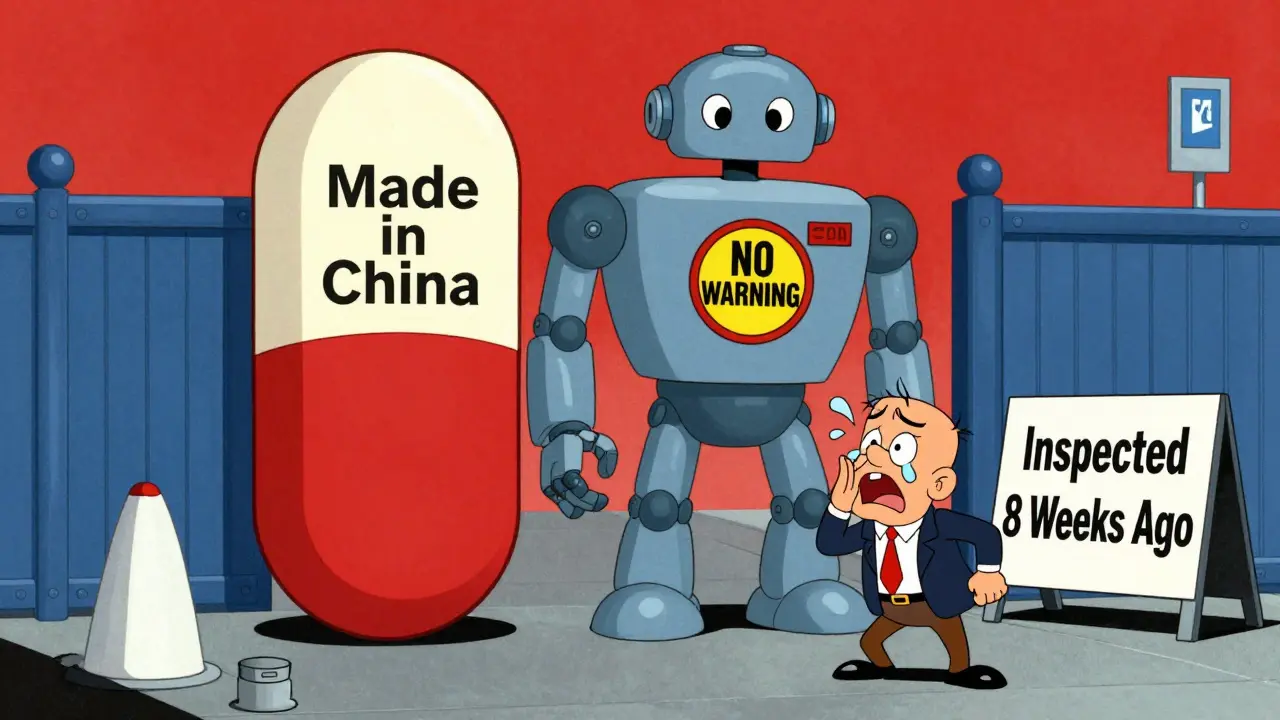
How Foreign Manufacturers Are Adapting
Companies are scrambling to prepare. A survey by the Parenteral Drug Association found 68% of foreign manufacturers expect compliance costs to rise 15-25%. Smaller factories, especially in India, are struggling. They don’t have the staff or budgets to hire quality auditors full-time. The advice from legal firms like McGuireWoods and White & Case is simple: act like you’re always being watched. That means:- Running mock inspections every quarter
- Keeping digital records that can’t be edited after the fact
- Training staff to answer questions without coaching
- Testing equipment daily, not monthly
- Documenting every deviation-even small ones
What Could Happen If You Don’t Comply
Refuse an FDA inspection? Your entire shipment gets blocked. No more drugs into the U.S. That’s not a warning. That’s a shutdown. The FDA can issue an import alert. That means every future shipment from your facility gets detained at the border until you prove it’s safe. It can take months. And during that time, your customers-hospitals, pharmacies, patients-start looking elsewhere. In 2025, over 200 foreign facilities received warning letters for CGMP violations. Most had to retrain staff, upgrade equipment, or shut down lines. Some lost FDA approval entirely. And once you’re on the FDA’s blacklist, getting back in is nearly impossible.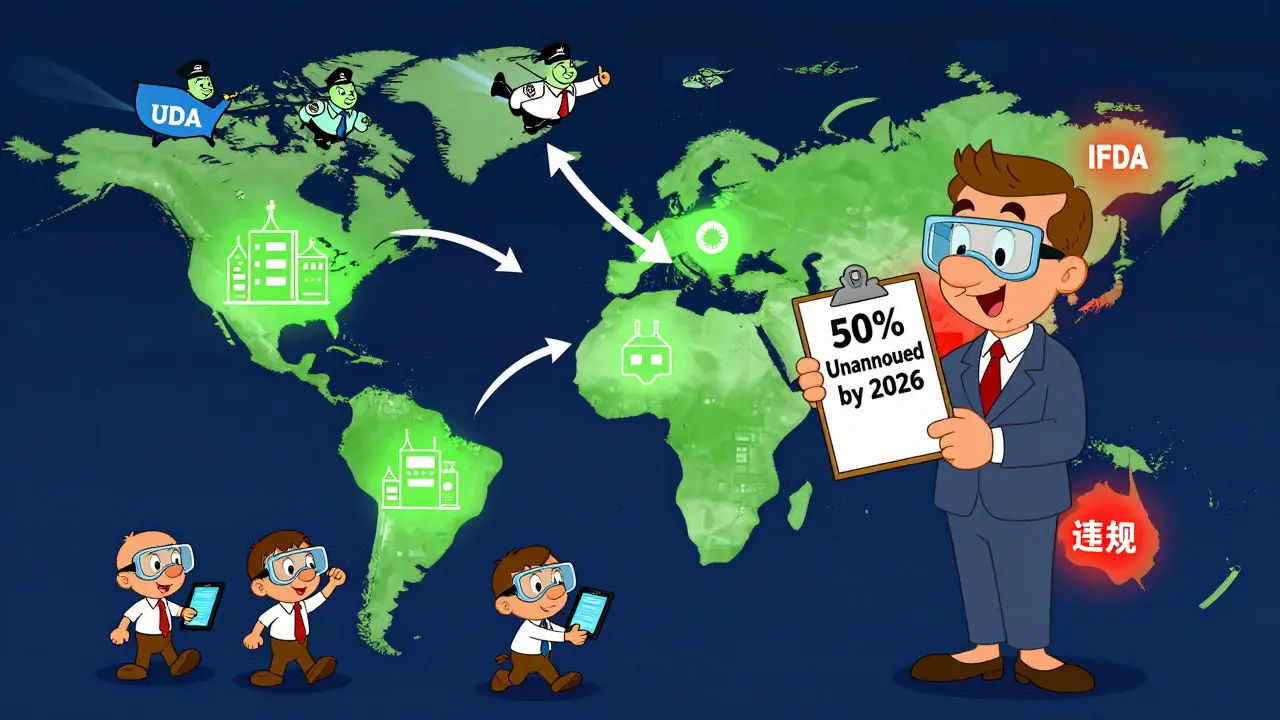
Could the U.S. Adopt the EU’s Model?
The European Union doesn’t rely on surprise inspections alone. Every batch of medicine leaving a plant must be certified by a “Qualified Person”-a trained professional who physically signs off on its safety. That person is legally responsible. If something goes wrong, they can be held accountable. Brookings Institution says the U.S. should try something similar. They propose requiring U.S.-based importers to name their own Qualified Person who verifies each batch meets standards before it crosses the border. Right now, the FDA checks the factory. But no one checks the importer’s paperwork. It’s a big shift. But it could cut violations by 30-40%, according to Brookings. And it would put responsibility where it belongs: with the company bringing the drugs into the U.S.What This Means for Patients
You take generic drugs because they’re cheaper. But cheap doesn’t mean unsafe. The goal isn’t to scare people. It’s to make sure the drugs you swallow work the same way every time. With better oversight, you’re less likely to get a pill that doesn’t dissolve properly. Or one made in a dirty room. Or a batch where the active ingredient was cut by 30% because someone falsified the test results. The FDA’s new approach isn’t about punishing foreign manufacturers. It’s about leveling the playing field. If you make a drug for Americans, you play by American rules. No exceptions.What’s Next? The Road to 2026
By mid-2026, the FDA expects to inspect at least half of all foreign generic drug plants without warning. They’ll also start sharing inspection data with global partners more openly. That means if Japan finds a problem at a plant in China, the FDA will know about it within days-not months. Some experts warn of short-term disruptions. Evaluate Pharma predicts up to 20% of generic drug supplies could be delayed as factories adjust. But long-term? Supply chains will be more reliable. More transparent. Safer. The bottom line: the era of foreign manufacturers getting a pass is over. The FDA is no longer asking for compliance. They’re demanding it. And if you’re making drugs for the U.S. market, you’d better be ready.Are foreign-made generic drugs safe?
Yes-if they meet FDA’s CGMP standards. Most foreign-made generics are safe and effective. But before 2025, inspection gaps allowed some non-compliant facilities to slip through. The FDA’s new unannounced inspection policy is designed to catch those problems before drugs reach patients. Today, the system is stronger than ever.
Why does the FDA inspect foreign plants less often than U.S. ones?
It wasn’t supposed to be that way. Historically, the FDA had fewer inspectors and more travel restrictions, so they scheduled visits far in advance. That created a loophole. Facilities had time to prepare. Starting in 2025, the FDA is rapidly increasing unannounced inspections to match domestic levels, with a goal of 50% of foreign inspections being surprise visits by mid-2026.
What happens if a foreign factory refuses an FDA inspection?
Refusing an inspection triggers an automatic import alert. All drugs from that facility are blocked at the U.S. border. The facility must fix the issue and prove compliance before shipments resume. This can take months-and many companies never recover. Refusal is one of the fastest ways to lose access to the U.S. market.
Do U.S. companies still use foreign manufacturers?
Yes-over 80% of active pharmaceutical ingredients and 40% of finished generic drugs come from abroad, mostly India and China. U.S. companies rely on them because they’re cost-effective. But now, they’re required to ensure their overseas partners meet the same standards as U.S. factories. Many are investing in audits, training, and real-time compliance systems to stay compliant.
How can patients know if their generic drug is made safely?
Patients can’t directly check a facility’s inspection status. But they can trust that the FDA now has a much stronger system in place. All approved generics must meet the same standards, no matter where they’re made. If a drug is on the market, it has passed FDA review. The increased inspections mean fewer bad actors are slipping through the cracks.
Will foreign drug prices go up because of stricter inspections?
Possibly. Factories now spend more on training, equipment, and documentation. Some estimates suggest compliance costs could rise 15-25% for foreign manufacturers. That could lead to modest price increases over time. But the FDA says the cost of unsafe drugs-hospitalizations, lawsuits, lost trust-is far higher. Safety is the priority.