Inhaler Side Effect Prevention Calculator
Prevent Oral Thrush & Hoarseness
Learn how much your risk can decrease with proper technique. Based on the latest clinical evidence, these methods work together to reduce side effects significantly.
Your Risk Reduction
Based on your current technique
Your Risk Reduction
Based on your current technique
Using an inhaled corticosteroid every day can keep your asthma under control-but it can also leave you with a white, patchy tongue or a voice that sounds like you’ve been shouting all day. These aren’t rare side effects. They’re common. And they’re mostly preventable.
Why Your Inhaler Causes Oral Thrush
Inhaled corticosteroids like fluticasone, budesonide, and beclomethasone are designed to land in your lungs. But too often, they don’t make it that far. Instead, a good chunk of the medicine sticks to the back of your throat, your tongue, and the insides of your cheeks. That’s not a design flaw-it’s physics. The particles are too large to always reach deep into the airways. When that medicine sits there, it quietly weakens your local immune defenses. Normally, your mouth has harmless fungi called Candida living in it. But when steroids shut down your body’s ability to keep them in check, Candida grows out of control. That’s oral thrush: creamy white patches that look like milk curds. They can be scraped off, but underneath, the tissue is red and sore. You might feel a burning sensation, lose your sense of taste, or notice it hurts to swallow. The risk goes up with dose. If you’re on more than 800 mcg per day of beclomethasone equivalent, your chances of getting thrush jump significantly. Older adults, people with diabetes (especially with HbA1c above 7.0%), and those with dry mouth are at higher risk too. Dry mouth means less saliva, and saliva is your mouth’s natural defense system.Why Your Voice Gets Hoarse
Hoarseness is another direct result of medicine landing where it shouldn’t. When corticosteroid particles touch your vocal cords, they cause irritation and swelling. You don’t need to have an infection-just contact. That’s why hoarseness often hits within minutes after using your inhaler. Your voice might sound raspy, weak, or lower than usual. It can last for hours, sometimes even a full day. This isn’t just annoying. For singers, teachers, or anyone who relies on their voice, it can be frustrating enough to make them skip doses. And that’s dangerous. Skipping your inhaler because of hoarseness puts you at risk for asthma flare-ups. The good news? You can reduce this side effect without stopping your medication.The Two Most Effective Prevention Tactics
There are two proven ways to stop these side effects before they start: rinse and spit, and use a spacer. Rinsing your mouth with water right after using your inhaler cuts your risk of oral thrush by 60-70%. It’s that simple. But it’s not just a quick swish. You need to gargle, swish, and spit. Don’t swallow the water. Spit it out. Do this every single time-morning, night, after every puff. Even if you’re using a rescue inhaler during an attack, rinse when you can. If you’re too breathless, do it as soon as you catch your breath. A spacer is a plastic tube that attaches to your inhaler. It holds the medicine in a chamber so you can breathe it in slowly. Without a spacer, most of the dose hits your mouth and throat. With one, only the tiny particles that can reach your lungs make it through. Studies show that using a spacer reduces oral deposition by up to 80%. That means less medicine sitting on your tongue, less irritation on your vocal cords, and far fewer cases of thrush. Some people think using a spacer makes rinsing unnecessary. But experts disagree. The 2025 review in Healthcare (Basel) says both work together. Spacers reduce the amount of medicine that reaches your mouth. Rinsing removes what’s left. Use both.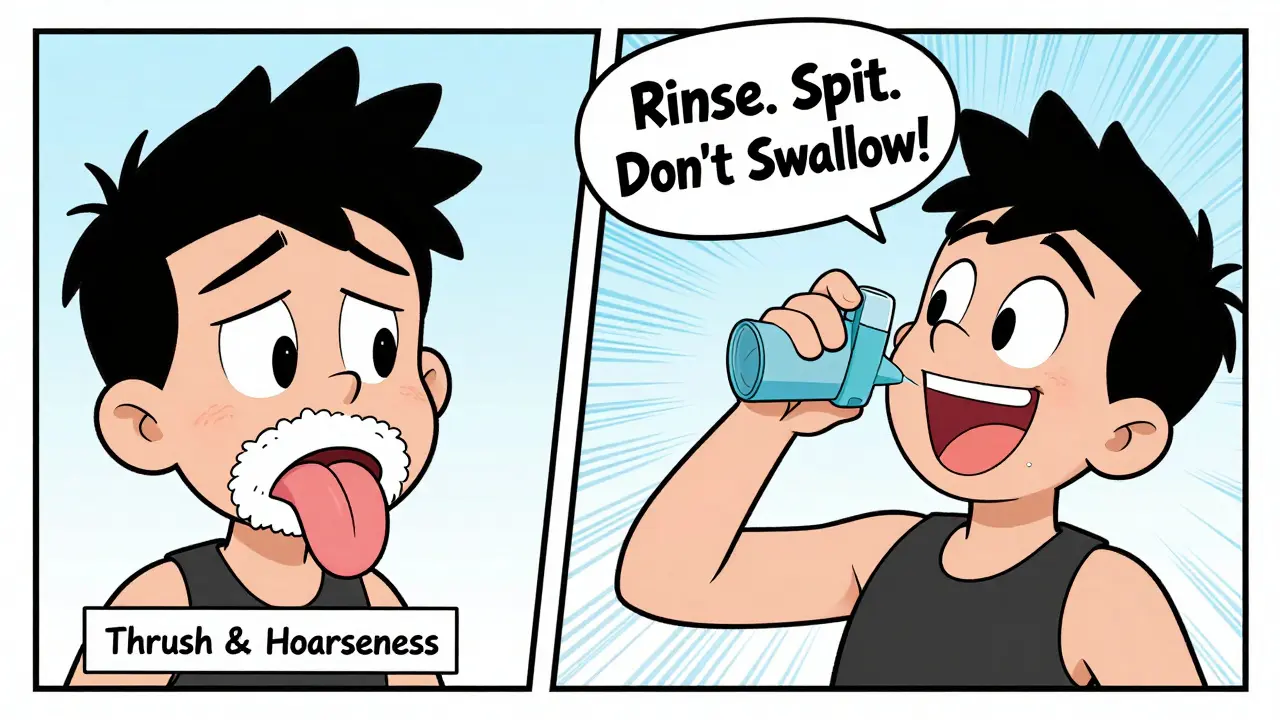
How to Use a Spacer Correctly
Not all spacers work the same. To get the full benefit:- Attach the spacer to your inhaler.
- Shake the inhaler well.
- Breathe out fully, then seal your lips around the spacer mouthpiece.
- Press the inhaler once to release one puff into the spacer.
- Breathe in slowly through your mouth for 4-5 seconds.
- Hold your breath for 10 seconds.
- Breathe out slowly.
- Wait 30 seconds before taking another puff, if needed.
What to Do If You Already Have Thrush
If you see white patches in your mouth, don’t panic. Oral thrush is treatable. Your doctor can prescribe a simple antifungal-usually nystatin oral suspension (a liquid you swish and swallow) or clotrimazole troches (lozenges that dissolve slowly in your mouth). Treatment takes 7-14 days. But here’s the catch: thrush often comes back if you don’t fix the cause. If you keep using your inhaler the same way, the thrush will return. That’s why treatment alone isn’t enough. You need to combine it with rinsing and spacer use. Some people try rinsing with a diluted antifungal like amphotericin B (a 1:50 mix with water) as a preventive rinse. This works, but it’s not routine. Only use it if your doctor recommends it. For most people, plain water is enough.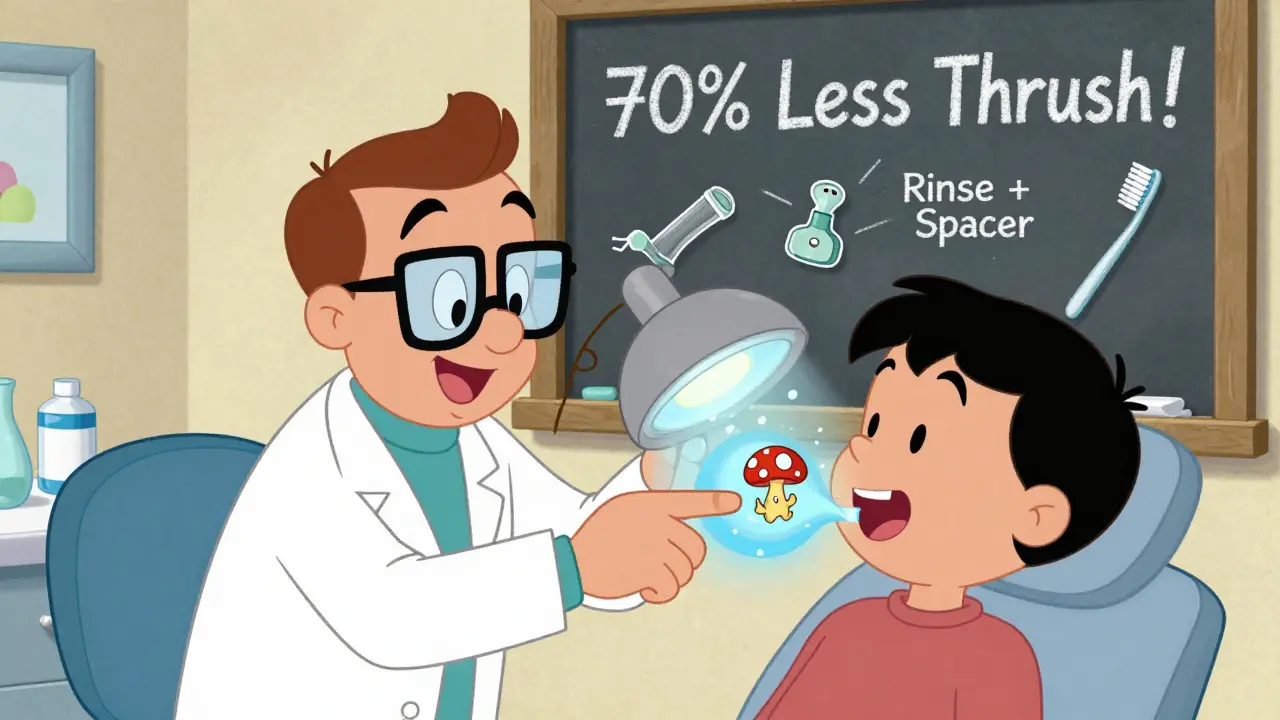
Other Helpful Tips
- Brush your teeth after using your inhaler. This removes residue and stimulates saliva flow. It’s especially helpful if you use your inhaler at night.
- Keep water by your bed. If you use your inhaler before sleep, forgetfulness is the #1 reason people skip rinsing. A glass of water on your nightstand makes it automatic.
- Check your mouth weekly. Look in the mirror. Lift your tongue. Check your cheeks. Early detection means faster treatment.
- Ask your doctor about newer inhalers. Ciclesonide and mometasone have lower oral deposition rates. If you’re on a high dose and keep getting thrush, ask if switching could help.
- Talk to your dentist. Many dentists now screen for steroid-related oral changes. Tell them you use an inhaled corticosteroid. They can spot early signs you might miss.
Why So Many People Still Get Thrush
You’d think this would be simple. Rinse. Use a spacer. Done. But studies show only 45% of patients rinse after every use. In one 2022 survey, 65% forgot to rinse at night. Why? Because it’s easy to forget. Because it feels like an extra step. Because you’re tired. Because you think the spacer makes it unnecessary. The truth? Prevention only works if you do it every time. One missed rinse doesn’t guarantee thrush. But 10 missed rinses? That’s a recipe for infection. The best advice comes from people who’ve been there. One user on Asthma.net said: “I got thrush twice in five years. Then I started rinsing, gargling, swishing, and spitting after every puff. I haven’t had it since. Takes 30 seconds. Worth it.”What’s Changing in the Future
The industry is starting to respond. New inhalers are being designed with built-in spacers. Some have coatings that reduce how much medicine sticks to the mouth. Smart inhalers are being tested-they track when you use them and even remind you to rinse. In the UK, pilot programs are pairing respiratory nurses with dental hygienists to manage ICS patients together. Early results show a 35% drop in oral complications. That’s the future: care that connects your lungs to your mouth. For now, the tools you need are already here. You don’t need a new device. You don’t need a new prescription. You just need to rinse after every puff. Use a spacer. Brush your teeth. Check your mouth. Do it every time. It’s not glamorous. But it’s the only way to keep your lungs healthy-and your voice and mouth free of side effects.Can I rinse with mouthwash instead of water?
You can, but plain water is best. Alcohol-based mouthwashes can dry out your mouth, which increases your risk of thrush. If you want to use mouthwash, choose an alcohol-free version, but don’t rely on it as your only rinse. Water is free, safe, and proven.
Do I need to rinse if I use a dry powder inhaler?
Yes. Dry powder inhalers (DPIs) like Pulmicort Flexhaler or Asmanex still leave residue in your mouth. They’re better than metered-dose inhalers without spacers, but they don’t eliminate oral deposition. Always rinse and spit after use, no matter what type of inhaler you have.
Will switching inhalers get rid of my hoarseness?
It might help. Ciclesonide and mometasone are designed to deposit less in the throat. But switching alone won’t fix it if you’re not rinsing or using a spacer. The best results come from combining a lower-deposition inhaler with good technique. Talk to your doctor about your options.
Can oral thrush spread to my lungs?
No. Oral thrush is a local fungal infection in the mouth and throat. It doesn’t spread to the lungs. But if you’re immunocompromised (e.g., from long-term steroid use or other conditions), you’re at higher risk for systemic fungal infections. That’s rare and different from oral thrush. If you have trouble swallowing, fever, or chest pain, see your doctor immediately.
Is it safe to use a spacer with a rescue inhaler like albuterol?
Yes. Spacers work with rescue inhalers like albuterol. In fact, they make them more effective by delivering more medicine to your lungs and less to your throat. If you use a rescue inhaler often, a spacer helps reduce throat irritation and hoarseness too. Keep one handy for emergencies.
How long does it take for hoarseness to go away after I start rinsing?
Most people notice improvement within a few days. If your voice stays hoarse for more than two weeks after you start rinsing and using a spacer, talk to your doctor. You might need to check for other causes, like acid reflux or vocal cord damage. But in most cases, hoarseness clears up quickly once the steroid stops coating your vocal cords.