
If you’ve had a stubborn, itchy rash that keeps coming back no matter what cream you use, you’re not alone. About 13.7 million workers in the U.S. deal with allergic contact dermatitis every year. It’s not just dry skin or bad hygiene-it’s your immune system reacting to something touching your skin. And most people have no idea what it is.
What’s Really Causing Your Rash?
Allergic contact dermatitis isn’t an immediate reaction like a peanut allergy. It takes days. That’s why it’s so easy to miss. You use a new lotion, wear a new watch, or start using a different shampoo-and two or three days later, your skin turns red, flakes, blisters, or burns. By then, you’ve already washed it off, moved on, and blamed your soap, your laundry detergent, or even stress. The real culprit? A tiny chemical called a hapten. These are low-weight molecules in everyday products that sneak past your skin’s barrier, stick to your proteins, and trick your immune system into thinking they’re invaders. Your body sends T-cells to attack. That’s what causes the inflammation. And once your immune system learns to recognize it, you’ll react every time you touch it again. The most common trigger? Nickel. It’s in jewelry, belt buckles, zippers, phone cases, and even some eyeglass frames. Studies show 14.7% of people tested for contact allergies react to nickel. In women, that number jumps to 17.4%. That’s why your earlobes itch after wearing earrings, or your wrist turns red under your watchband. Other frequent offenders include:- Thimerosal (a preservative in some eye drops and vaccines)
- Cobalt chloride (found in metal alloys, cement, and some cosmetics)
- Fragrance mix (hidden in perfumes, lotions, shampoos-even "unscented" products)
- Balsam of Peru (used in flavorings, cosmetics, and medicinal creams)
- Cocamidopropyl betaine (a foaming agent in shampoos and body washes)
How Do You Know What’s Triggering It?
You can’t guess your way out of this. The only reliable way to find your allergen is through patch testing. It’s not a needle. It’s not a blood test. It’s small patches taped to your back, loaded with 29 common allergens, left on for 48 hours, then checked again at 96 hours. The standard test is called the TRUE Test. It’s used in clinics worldwide. But here’s the catch: it only tests for 29 allergens. There are thousands of potential triggers in everything from your toothpaste to your yoga mat. If your rash doesn’t match any of the standard 29, you might get a false negative. That’s why experts now recommend expanded patch testing for people with chronic or unexplained rashes. Some clinics now test up to 100 allergens, including ones tied to hair dyes, industrial chemicals, or even ingredients in green cleaning products. Dr. Matthew Zirwas, a leading dermatologist in Ohio, says patch testing changes how people manage their condition in 60-70% of cases. One Reddit user, "EczemaWarrior87," spent five years with hand eczema until patch testing revealed an allergy to cocamidopropyl betaine. Once they switched to a sulfate-free, fragrance-free cleanser, their skin cleared up completely. But it’s not perfect. Another user, "RashQueen2023," had a negative result on the standard test-only to later discover a formaldehyde allergy through expanded testing. It cost her $350 out-of-pocket.What Happens After the Test?
Finding the allergen is only half the battle. Avoiding it is the other half. And that’s harder than it sounds. Fragrance is everywhere. Even "unscented" products can contain masking fragrances to cover up chemical smells. Nickel hides in stainless steel, cheap jewelry, and the buttons on your jeans. Cobalt shows up in blue pigments used in paints and cosmetics. Balsam of Peru is in cinnamon, vanilla, and even some teas. That’s where the Contact Allergen Management Program (CAMP) comes in. Run by the American Contact Dermatitis Society, CAMP gives you a personalized list of products that are safe for your specific allergens. Their database, called the Contact Allergen Replacement Database (CARD), now includes over 18,000 consumer products-from shampoos to dish soaps to makeup. One 2023 survey of 1,247 patients found that 82% saw significant improvement after avoiding their identified allergens. But 47% struggled to find safe alternatives. Why? Because labels lie. Ingredients like "parfum" or "fragrance" can hide dozens of chemicals. And manufacturers aren’t required to list them individually in the U.S.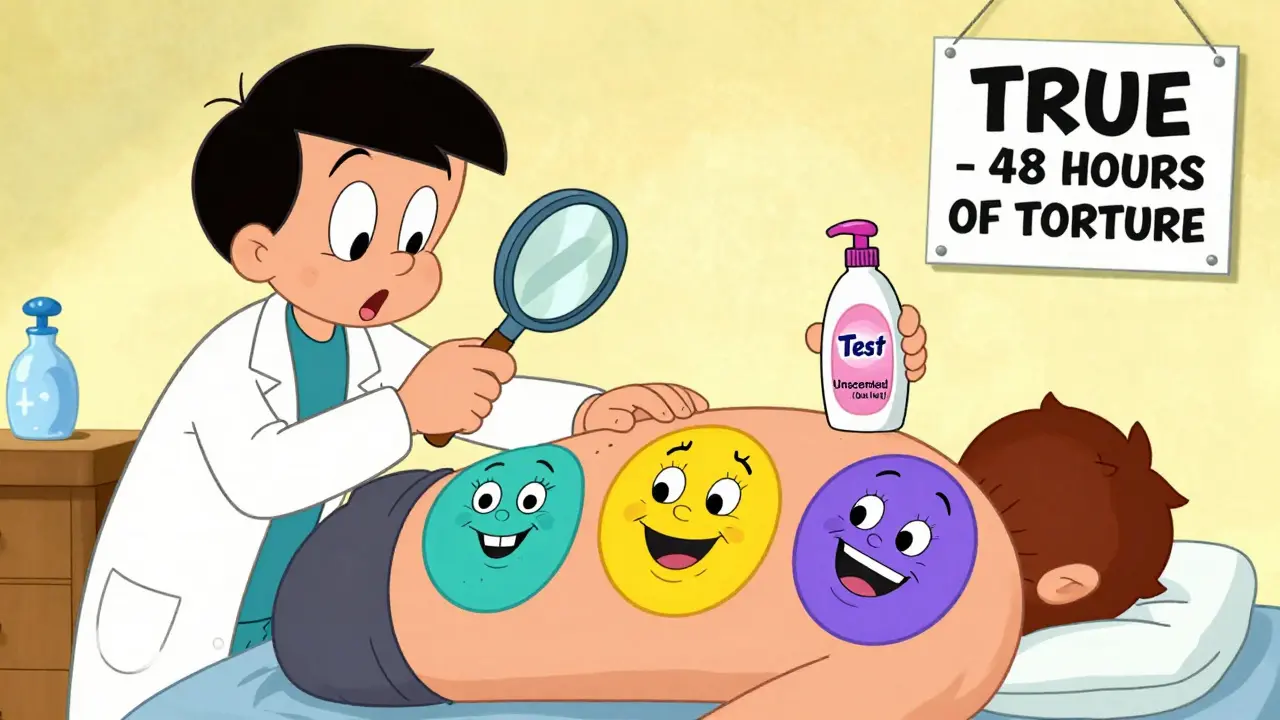
How to Avoid Allergens in Real Life
Here’s how to make avoidance work:- Read labels like a detective. Look for the exact names of your allergens-not just "fragrance" or "chemicals." Use the CARD database to find safe brands.
- Switch to hypoallergenic, fragrance-free products. Brands like Vanicream, Cetaphil, and Aveeno Free & Clear are often safe, but always double-check the ingredient list.
- Test new products on a small patch of skin first. Apply a dab to your inner forearm for three days. If nothing happens, it’s probably safe.
- Wear gloves. If you work with cleaners, chemicals, or even wet dishes, use cotton-lined gloves. Latex and nitrile can contain allergens too.
- Replace metal accessories. If nickel is your trigger, switch to titanium, surgical steel, or plastic jewelry. Use clear nail polish on the back of watchbands to create a barrier.
- Be careful with cosmetics. Avoid products with balsam of Peru, tree nut oils, or essential oils if you’re sensitive. Even "natural" doesn’t mean safe.
Workplace Risks and What to Do
If your job involves constant skin exposure, you’re at higher risk. Hairdressers (42.3%), healthcare workers (25.7%), and construction workers (18.9%) have the highest rates of contact dermatitis. In the EU, employers are required to identify and reduce allergen exposure under REACH regulations. In the U.S., OSHA doesn’t have the same rules. That means if you’re a nurse or a mechanic with a rash, you might need to push your employer for safer alternatives. Talk to your dermatologist about writing a letter to your employer. Many companies will switch to fragrance-free soaps, provide barrier creams, or allow you to use your own tools to avoid cross-contamination.
What’s Changing in 2025?
The field is evolving. By Q3 2025, the TRUE Test will expand to 80 allergens, adding new triggers from electronics (like acrylates in screen protectors) and "green" cosmetics (like plant-based preservatives). Researchers are also exploring blood tests. Dr. Jeanne Duus Johansen’s 2024 study found that IL-18 levels in the blood correlate strongly with the severity of contact dermatitis. That could mean one day, instead of waiting 96 hours for a patch test, you might get a simple blood draw. But for now, patch testing remains the gold standard. Dr. Howard Maibach says it’s irreplaceable. No lab test can yet match its real-world accuracy.What If You Still Can’t Find the Cause?
Sometimes, you’ll test negative but still react. That could mean:- You need expanded testing
- You’re reacting to a combination of chemicals
- You have irritant dermatitis, not allergic
- Something in your environment-like water quality or laundry detergent-is triggering it
- Rule out other skin conditions (like psoriasis or fungal infections)
- Map out your daily exposures-what do you touch every day?
- Get patch tested
- Eliminate the allergen for 2-4 weeks and watch for improvement
Final Thought: You’re Not Imagining It
If your skin reacts, it’s not in your head. It’s not stress. It’s not bad luck. It’s a real, measurable immune response to a chemical you’re touching every day. And with the right testing and avoidance, you can take control. The data is clear: 76% of patients say knowing the exact cause reduces their anxiety. 78% improve with CAMP-guided avoidance. And nickel allergy rates have dropped 25% in Europe since laws banned it in jewelry. You don’t need to live with a rash. You just need to know what’s causing it-and how to walk away from it.Can contact dermatitis go away on its own?
It can, but only if you stop touching the allergen. If you keep using the same soap, wearing the same watch, or handling the same tools, the rash will return. Avoidance is the only cure. Without it, the condition often becomes chronic and harder to treat.
Is patch testing painful?
No. The patches are taped to your back and don’t break the skin. You might feel mild itching or burning if you’re allergic to one of the substances, but it’s not painful. The biggest discomfort is having to keep your back dry and not scratching for four days.
Can I do patch testing at home?
No. Patch testing requires medical supervision. The allergens are potent, and misreading results can lead to false negatives or unnecessary reactions. Only trained dermatologists or allergists should perform and interpret these tests.
Are natural or organic products safer for contact dermatitis?
Not necessarily. Many natural products contain plant extracts like tea tree oil, lavender, or balsam of Peru-all common allergens. "Organic" doesn’t mean hypoallergenic. Always check the ingredient list, even for natural brands.
How long does it take to see improvement after avoiding an allergen?
Most people notice improvement within 2-4 weeks. Severe cases may take up to 6-8 weeks. If you don’t see changes after a month, revisit your doctor. You might need expanded testing or a different approach.
Can I develop new allergies over time?
Yes. Once your skin is sensitized, it becomes more reactive. You might develop allergies to new chemicals you weren’t sensitive to before. That’s why avoiding known triggers and using gentle products long-term is so important.
Does insurance cover patch testing?
Most insurance plans in the U.S. cover patch testing if ordered by a dermatologist. However, expanded testing or follow-up visits may require prior authorization. Always check with your provider before scheduling.





