If there’s one thing more annoying than stubborn skin rashes, it’s trying endless creams only to find nothing really works. Lotrisone sits in a unique spot: it tackles angry fungal infections while fighting stubborn inflammation at the same time. But how did we end up with such a two-in-one cream, and is it really a magic fix?
What is Lotrisone and How Does It Work?
Lotrisone isn’t just any ointment you grab at the chemist. It’s what dermatologists call a combination therapy, packaging two mighty ingredients—clotrimazole and betamethasone dipropionate—into one tube. Clotrimazole is an antifungal, known for zapping fungi that cause ringworm, athlete’s foot, and jock itch. Betamethasone is a corticosteroid, calling off the body’s inflammatory response so swelling, redness, and itching back down.
Why a combo? For plenty of people, a fungal infection doesn’t just itch—it gets inflamed and makes skin look red and cracked. The antifungal nukes the infection, while the steroid soothes your skin so you don’t claw it to shreds overnight. This makes Lotrisone a go-to for short-term rescue, not a daily staple. With this cream, you treat the visible infection, not just the symptoms.
Fun fact: When used as directed, most fungal infections start clearing up within a week. A double-blind study from 2017 showed up to 85% of patients with tinea cruris (jock itch) saw nearly complete improvement after only two weeks using Lotrisone. Quick wins are rare with rashes, but with this cream, that’s exactly what people hope for.
Common Uses and When to Reach for Lotrisone
So, who really needs Lotrisone? It’s most often prescribed for tinea pedis (athlete’s foot), tinea cruris (jock itch), and tinea corporis (body ringworm)—all fungal skin infections that can get especially red, crusty, or swollen. Got an angry patch of eczema and wondering if Lotrisone is right? Hold off. This isn’t a basic steroid cream for eczema, psoriasis, or plain irritated skin. Lotrisone specifically hits infections where fungus and inflammation meet.
Pediatricians often avoid prescribing it for children under 17, as their skin absorbs topical steroids more easily, leading to side effects. Pregnant or breastfeeding? There’s not enough solid data to say it’s safe, so always check with a doctor.
Typical prescriptions go like this: apply a thin layer once or twice a day to clean, dry skin, and rub it in until it vanishes. Don’t slap it on like it’s body lotion—a little goes a long way. Almost every instruction says stop after two weeks for groin and body, and four weeks for feet. Why? Prolonged use increases side effects (more on that soon).
Unlike over-the-counter creams, Lotrisone needs a prescription in the UK and most countries. Don’t try sneaking it onto your eczema patches or mystery rashes; spotting the right culprit makes all the difference. Think you’ve got an infection? Ask your GP or pharmacist to be sure, and don’t diagnose from internet photos.
Known Side Effects and Warnings
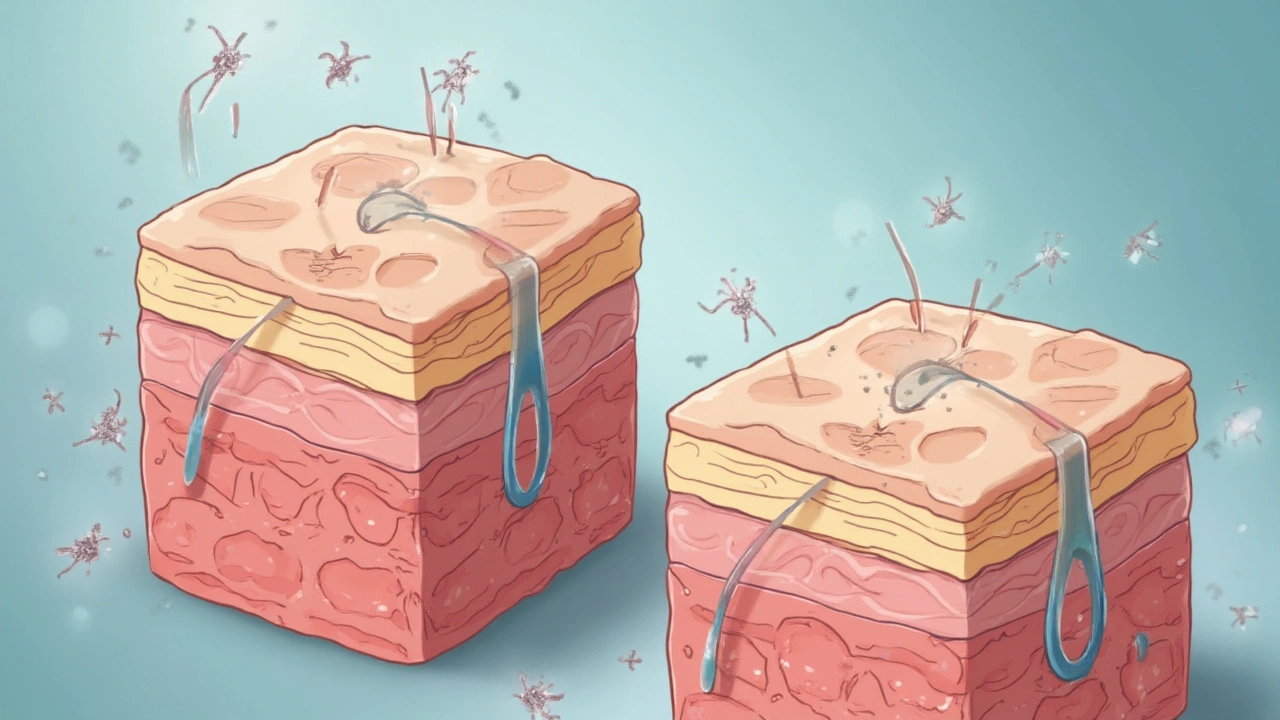
Medications that work fast can also bite back if used carelessly. Lotrisone’s biggest risk comes from the steroid side: betamethasone can thin your skin, spur stretch marks, lighten pigment, or even create “steroid acne” if you use it too often. Around 4% of people using it for over two weeks report increased skin fragility, so keep an eye out. Some feel a burning or stinging sensation the first few times it’s applied—that’s usually normal and fades fast.
Worried about allergies? Rare, but not impossible. Watch for swelling, rash spreading, trouble breathing, or hives—and get medical help right away if those hit. Using it on your face, underarms, or groin ups your risk of side effects, since skin is thinner there.
There’s another hitch: using Lotrisone too long can actually worsen or spread the infection. Why? Long-term steroid use suppresses your immune response, which lets fungi dig in deeper. If your rash isn’t getting better after one week, or comes roaring back after you stop, get checked out again.
People with diabetes or immune problems need to be extra cautious. Fungal infections can be stubborn and harder to treat, and there’s a slight uptick in skin atrophy risk. For the curious, here’s a quick look at reported side effects from a review of UK pharmacy data (2022):
| Side Effect | Frequency (%) |
|---|---|
| Skin thinning | 4 |
| Burning/stinging | 7 |
| Stretch marks | 2 |
| Hypopigmentation | 1.5 |
| Secondary infection | 0.5 |
Tips for Safe and Effective Use
You want good results, not surprises. Here are some down-to-earth tips for using Lotrisone properly:
- Always wash your hands before and after applying the cream. Fungus and bacteria love dirty hands.
- Clean and dry the area thoroughly before use. Remember, fungus thrives in damp spots.
- Apply a thin layer—don’t glob it on. Too much is not better and actually increases risks.
- Don’t cover the treated area with bandages unless your doctor says to. It boosts absorption and side effects.
- If you accidentally get it in your eyes, rinse with water immediately and contact a doctor if irritation persists.
- Finish the full treatment course, even if skin looks better partway through. Stopping early invites the fungus back.
- Store the cream at room temperature; avoid heat and moisture, like bathrooms with constantly steaming showers.
- If you miss a dose, just use it as soon as you remember, unless it’s close to the next scheduled dose. In that case, skip it. Double dosing isn’t safe.
Thinking of sharing your leftover tube with someone who looks a bit spotty? Don’t. Different rashes mean different issues, and steroids can make some rashes worse, not better.
Another pro tip: mark your calendar when you start applying Lotrisone. It’s easy to lose track of time, and using it longer than prescribed just increases the chance of skin issues and wonky pigmentation.

When to See a Doctor and Alternative Treatments
If your rash isn’t improving after the recommended time, gets worse, or spreads to new spots, get checked. You might need a different antifungal or a deeper look into what’s really causing your irritation. Rashes that blister, ooze, or hurt a lot are worth flagging early.
Lotrisone isn’t for every fungal infection. If you’ve got nail infections (fungal toenails—joy!), or a scalp issue, you’ll need a different medication or even oral antifungals. Sometimes, a GP will prescribe plain clotrimazole or miconazole without the steroid if inflammation isn’t a big problem. This is safer for long-term use and areas where steroids could thin delicate skin.
If your skin is simply dry or itchy without a true fungal infection, moisturizers and gentle steroid creams—without antifungals—do the job. Using Lotrisone on eczema or dermatitis without a fungal culprit can backfire, letting the wrong bugs take over.
So, as much as Lotrisone brings relief for the right condition, it can cause trouble in the wrong hands—or on the wrong rash. If you’re ever in doubt, a quick trip to the doctor or pharmacist saves time, hassle, and itch (or worse) down the road.
If you’re dealing with recurring athlete’s foot or jock itch, think prevention too: dry your feet well, rotate your socks, and avoid sharing towels. Lotrisone helps kill the infection fast, but smart habits keep it from returning.
To sum up, Lotrisone stands out for fungal skin infections topped with angry redness—but use it wisely, finish your course, and don’t get creative. If something doesn’t feel right, your local dermatologist or GP can steer you in the right direction.