When you pick up a generic pill at the pharmacy, you expect it to work just like the brand-name version. That’s not luck-it’s the result of strict bioequivalence studies required by the FDA. These studies are the backbone of the generic drug approval process, ensuring that a cheaper version of a drug delivers the same effect, safety, and performance as the original. But what exactly does the FDA demand before approving a generic drug? And why do some applications get rejected while others sail through?
What Bioequivalence Really Means
Bioequivalence isn’t about looking the same or tasting the same. It’s about how your body handles the drug. The FDA defines it as the absence of a significant difference in the rate and extent to which the active ingredient becomes available at the site of action. In plain terms: if you take two versions of the same drug-one brand, one generic-they must release the same amount of medicine into your bloodstream at roughly the same speed.
This isn’t just theory. It’s backed by decades of data and regulation. Since the 1984 Hatch-Waxman Act, the FDA has required generic manufacturers to prove bioequivalence before selling their products. Without this proof, a drug can’t be approved, no matter how cheap or well-made it seems.
The Two Requirements: Pharmaceutical and Bioequivalence
Before bioequivalence even comes into play, the generic must be pharmaceutically equivalent to the brand-name drug. That means:
- Same active ingredient
- Same dosage form (tablet, capsule, injection, etc.)
- Same strength
- Same route of administration (oral, topical, IV, etc.)
If those match, the FDA moves to the next step: proving bioequivalence. This is where the real science kicks in.
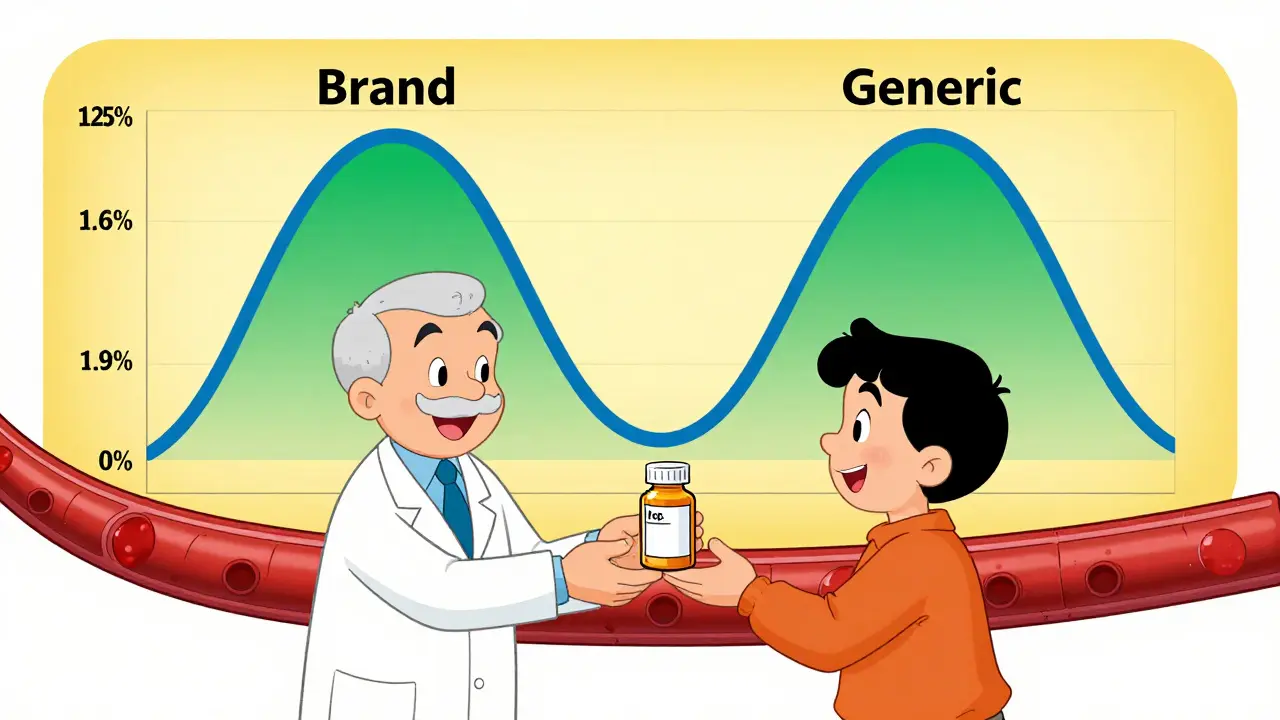
How Bioequivalence Is Measured: AUC and Cmax
The FDA doesn’t guess whether two drugs behave the same. It measures. Specifically, it looks at two key metrics from blood samples taken over time:
- AUC (Area Under the Curve): This shows the total amount of drug absorbed over time. Think of it as the drug’s overall impact on your body.
- Cmax (Maximum Concentration): This tells you how high the drug spikes in your blood. It reflects how fast the drug kicks in.
For approval, the 90% confidence interval for the ratio of these values between the generic and the brand-name drug must fall between 80% and 125%. This is known as the 80/125 rule. It’s been in place since 1992 and still holds today.
For example: If the brand-name drug delivers an AUC of 100 units, the generic must deliver between 80 and 125 units. Same for Cmax. If it’s outside that range, the FDA rejects the application.
Who Gets Tested? And How?
Most bioequivalence studies involve 24 to 36 healthy volunteers. They’re given either the generic or the brand-name drug in a crossover design-meaning half take the generic first, then switch to the brand, and vice versa. This controls for individual differences in metabolism.
Studies are usually done under fasting conditions. But if the drug’s absorption is affected by food (like some antibiotics or cholesterol meds), a second study is required after a high-fat meal. The FDA calls this “fed and fasted” testing.
All samples are analyzed using validated lab methods. The lab must follow Good Laboratory Practice (GLP) rules, and samples must be stored and tracked properly. A single study can cost between $500,000 and $2 million. That’s why many companies try to avoid it-when they can.
When You Don’t Need a Human Study: Biowaivers
Not every generic needs a full clinical trial. The FDA allows biowaivers-approval without human testing-for certain low-risk products. These are based on the Q1-Q2-Q3 framework:
- Q1: Same active and inactive ingredients as the brand
- Q2: Same dosage form and concentration
- Q3: Same pH, solubility, and dissolution profile
Examples include:
- Topical solutions for skin or eye use (like antibiotic eye drops)
- Oral solutions with identical ingredients
- Inhalant anesthetics
For these, manufacturers submit in vitro data-like how fast the drug dissolves in a lab test-instead of running a human trial. This can cut development time by 6 to 12 months.
When the 80/125 Rule Isn’t Enough
Not all drugs play nice with the standard bioequivalence rule. Some are highly variable-meaning their absorption differs wildly from person to person. Others have a narrow therapeutic index, where even a small change in blood levels can cause serious side effects or make the drug useless.
For these, the FDA tightens the rules:
- Highly Variable Drugs (HVDs): The FDA uses scaled average bioequivalence (SABE), which adjusts the acceptance range based on how variable the drug is. This prevents unfair rejections.
- Narrow Therapeutic Index Drugs (NTIDs): Like warfarin or levothyroxine. Here, the 90% confidence interval must fall between 90% and 111%. That’s a much tighter window.
These special rules exist because a 10% difference in blood levels might be harmless for a painkiller-but deadly for an anticoagulant.
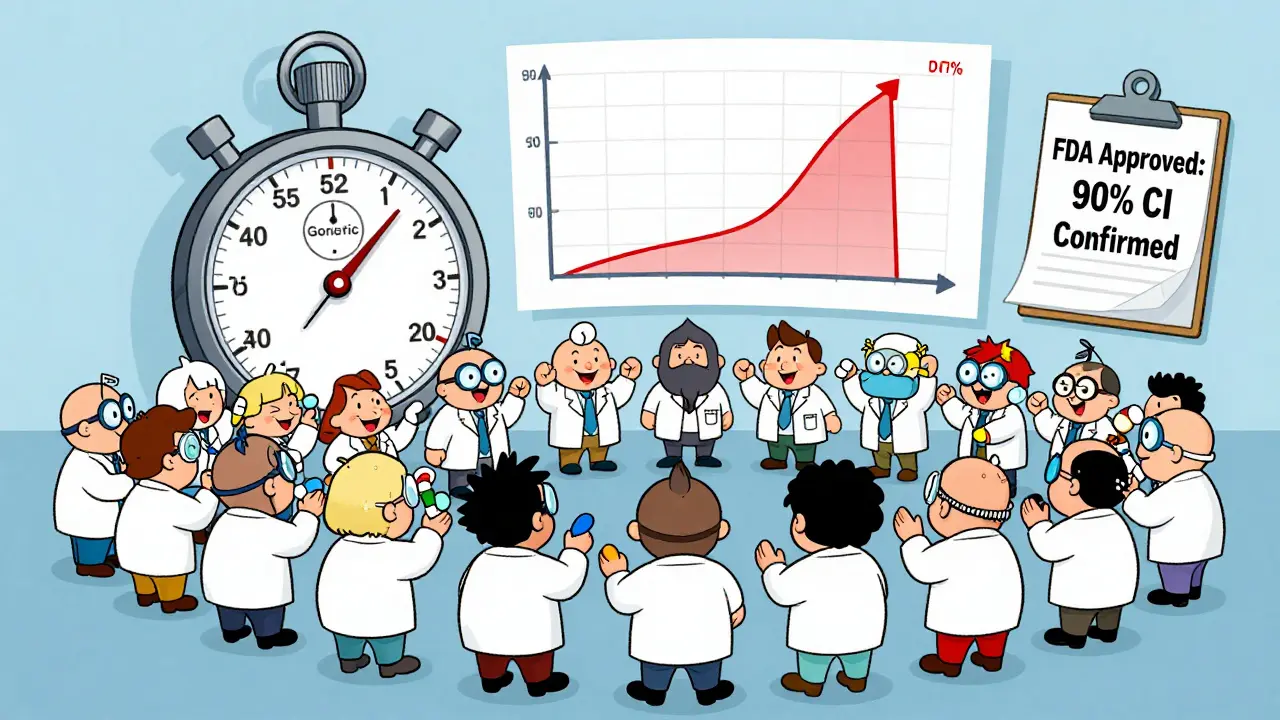
Why So Many Applications Get Rejected
Despite clear guidelines, the FDA approves only about 43% of generic drug applications on the first try. Why? Common mistakes include:
- Using outdated or unvalidated lab methods
- Too few volunteers or poor study design
- Not following the product-specific guidance (PSG)
- Missing documentation on sample handling or storage
Companies that follow the FDA’s product-specific guidances (there are over 2,100 of them) have a 68% first-time approval rate. Those that don’t? Just 29%. It’s not about quality-it’s about following the rules.
The Future: More Precision, Less Testing
The FDA is moving toward smarter, science-based approvals. New tools include:
- Physiologically Based Pharmacokinetic (PBPK) Modeling: Computer simulations that predict how a drug behaves in the body, reducing the need for human trials.
- In Vitro Permeation Testing (IVPT): For topical drugs, this measures how well the drug passes through skin layers-replacing animal or human tests.
- Advanced Dissolution Testing: More precise lab methods to mimic how the drug breaks down in the gut.
The goal? Faster approvals without sacrificing safety. The FDA’s roadmap includes draft guidances for 45 complex products by mid-2024, including inhalers, transdermal patches, and injectable suspensions.
What This Means for You
When you fill a generic prescription, you’re not taking a gamble. You’re getting a drug that’s been tested under the same rigorous standards as the brand. The FDA doesn’t approve generics because they’re cheaper. They approve them because they’ve proven they work the same way.
And that’s why 90% of prescriptions in the U.S. are for generics-while they cost only 23% of what brand drugs do. The system works because the science behind it doesn’t cut corners.
What happens if a generic drug fails bioequivalence testing?
If a generic drug fails bioequivalence testing, the FDA issues a complete response letter outlining the deficiencies. The manufacturer can either fix the issues and resubmit, conduct new studies, or withdraw the application. Many companies revise their formulation or testing methods and reapply-sometimes after months or even years of work.
Can a generic drug be approved without any human testing?
Yes, for certain products. The FDA grants biowaivers for simple formulations like oral solutions, topical creams for local effect, and some inhalants-provided they meet strict Q1-Q2-Q3 criteria and demonstrate identical in vitro performance to the brand-name drug. This avoids unnecessary clinical trials while ensuring safety.
Why is the 80/125% range used instead of 90/110%?
The 80/125% range was chosen based on decades of pharmacokinetic data and statistical modeling. It balances real-world variability in human absorption with the need for therapeutic equivalence. A tighter range like 90/110% would exclude many safe and effective generics, especially for drugs with natural variability in absorption. The range has been validated across thousands of studies and remains scientifically sound.
Do bioequivalence studies test for side effects?
Not directly. Bioequivalence studies focus on how much and how fast the drug enters the bloodstream-not on side effects. However, because the active ingredient and its exposure are identical, the FDA assumes side effect profiles will match. Post-marketing surveillance and adverse event reporting catch any unexpected differences after the drug is on the market.
Are FDA bioequivalence standards the same as Europe’s?
Yes, largely. The FDA and the European Medicines Agency (EMA) have aligned on core bioequivalence standards, with 87% of requirements now matching. Both use the 80/125% confidence interval for most drugs and have similar rules for HVDs and NTIDs. This harmonization helps global manufacturers submit applications to both regions with fewer changes.