When you hear the word biosimilar, you might think it’s just another name for a generic drug. But that’s not true. Biosimilars aren’t like the generic pills you pick up for high blood pressure or cholesterol. They’re complex, living medicines made from living cells - not chemicals mixed in a lab. And the FDA doesn’t just slap a stamp on them like it does for generics. There’s a whole different system in place to make sure they’re safe and effective.
What Makes a Biosimilar Different From a Generic?
Generics are exact copies of small-molecule drugs. Take ibuprofen. The active ingredient is one simple chemical structure. Any manufacturer can replicate it, and the FDA checks that it’s the same molecule, dissolves the same way, and gets into the bloodstream at the same rate. Done. Biosimilars are nothing like that. They’re copies of biologic drugs - proteins, antibodies, or other large molecules made by living cells. Think of them like cloning a tree. Even if you take a cutting from the same parent tree, no two clones are perfectly identical. Tiny differences in how the cells grow, how sugars attach to the protein, or how it folds can change how it works in your body. That’s why the FDA doesn’t call them “identical.” They call them “highly similar.” And they have to prove there are no clinically meaningful differences in safety, purity, or potency compared to the original biologic. That’s the bar. Not perfect copy. Perfectly safe and effective copy.The FDA’s Step-by-Step Approval Process
The FDA doesn’t approve biosimilars with a single test. It’s a layered science puzzle. Here’s how it works:- Analytical Studies: This is where most of the work happens. Scientists use advanced tools - mass spectrometers, capillary electrophoresis, chromatography - to compare the biosimilar and the original drug molecule by molecule. They look at over 200 different characteristics: shape, charge, sugar chains, purity, stability. The goal? At least 95% similarity on most attributes. Some need 99%. This phase alone can take 10-12 months and cost $120-180 million.
- Animal Studies: If the analytical data looks good, they test in animals. Not always required, but often used to check for unexpected toxicity. The FDA can skip this if the science is solid enough.
- Human Studies: A small clinical trial, usually with 50-100 people. It’s not about proving the drug works better than the original - it’s about proving it works the same. Pharmacokinetics (how the body absorbs and processes it) and pharmacodynamics (how it affects the body) are measured. These are usually crossover studies - you get the original, then the biosimilar, or vice versa.
- Immunogenicity Testing: This is critical. Biologics can trigger immune reactions. Even a tiny change can make your body attack the drug. So they track immune responses for 6-12 months after treatment. No spikes in antibodies? Good. Any red flags? Back to the lab.
- Final Review: The FDA looks at everything together - the analytical data, animal results, human trials, manufacturing details. If the totality of evidence shows no clinically meaningful differences, they approve it.
Compare that to a generic drug. Generics need a single bioequivalence test - blood levels over time. Biosimilars need a full scientific dossier. It’s not just harder. It’s a different kind of science.
The FDA Purple Book: The Official List
The FDA doesn’t publish a simple list of approved drugs like it does for generics. Instead, it maintains the Purple Book. It’s the official directory of all licensed biologics and their biosimilars. Updated daily since early 2025, it’s searchable online and even has an API for developers. Each entry includes:- The reference biologic’s name and approval date
- Each biosimilar’s name and approval date
- Whether it’s designated as “interchangeable”
- Patent information submitted by the original drug maker
- Exclusivity periods and patent litigation status
As of October 2025, the Purple Book lists 387 reference biologics and 43 approved biosimilars. Only 17 of those 43 are labeled “interchangeable.” That’s a big deal.
What Does “Interchangeable” Actually Mean?
This is where things get even more specific. Not all biosimilars are created equal in the eyes of pharmacists and insurers. An “interchangeable” biosimilar has met an extra standard. It must show that switching back and forth between it and the original drug won’t increase risk or reduce effectiveness. That means:- Same clinical results in any patient
- No increased risk of side effects when you switch
- Ability to be substituted without the prescriber’s permission - just like a generic
Only 17 of the 43 approved biosimilars have this status. Why so few? Because proving interchangeability requires extra studies - often multiple switches between the two drugs in the same patient. It’s expensive. It’s time-consuming. And most manufacturers don’t see the payoff yet, since many states still require prescriber notification before substitution.
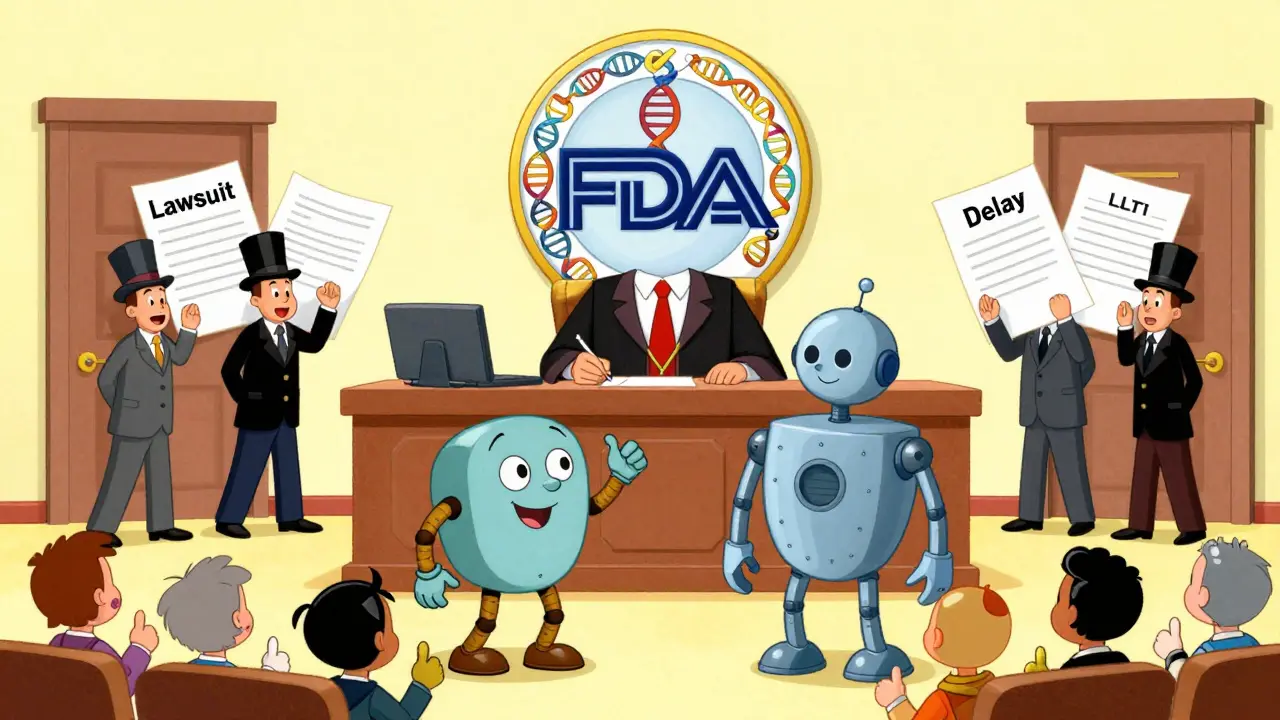
Why Are So Many Biosimilars Still Not on the Market?
You’d think with 43 approved, they’d be everywhere. But only 29 have actually launched. Why? Patent lawsuits. Big pharma companies hold hundreds of patents on their biologics - not just on the drug, but on how it’s made, stored, delivered. They use these to delay biosimilar entry. On average, it takes 11.3 months from FDA approval to market launch. Some take years. Payers - insurance companies and pharmacy benefit managers - also play a role. Many still prefer the original drug, even if the biosimilar is cheaper. They worry about patient confusion or rare side effects, even though data shows no difference. Real-world evidence from the FDA’s Sentinel Initiative shows biosimilars have the same safety profile as their reference products. Adverse events? 0.8 per 10,000 patients for biosimilars. 0.7 for originals. Statistically the same.
What’s Changing in 2025 and Beyond?
The FDA has been making big changes to speed things up:- Extrapolation: Since June 2025, if a biosimilar proves similarity in one condition (like rheumatoid arthritis), and the science is strong enough, it can be approved for other conditions the original drug treats - without running new clinical trials.
- AI for Analysis: Starting in early 2026, the FDA will pilot AI tools to review analytical data faster. This could cut review times by months.
- Complex Molecules: Antibody-drug conjugates and gene therapies are the next frontier. Only 3 applications have been submitted so far. None approved. New guidance is coming in late 2026.
These changes are already having an impact. The median development time for a biosimilar dropped from 6.8 years to 5.2 years. The FDA expects biosimilars to hit 30% of the biologics market by 2030 - up from 18% in 2024 - saving an estimated $250 billion.
Who’s Winning and Who’s Struggling?
The biggest success? Oncology. Drugs like rituximab and trastuzumab biosimilars now hold 65-75% of the market within 18 months of launch. Patients and doctors trust them. Payers push them. Savings are real. The biggest struggle? Autoimmune drugs like adalimumab. Even though biosimilars launched in 2023, they only captured 28% market share by mid-2025. Why? Prescriber hesitation. Fear of switching. Lack of clear guidelines for pharmacists. Manufacturers are frustrated too. A 2025 survey found 78% think the FDA’s analytical requirements are scientifically sound - but too costly and slow. Amgen told the FDA in 2024 that requiring 95-99% similarity on every single attribute - even minor ones - adds millions in cost without improving safety. Patient advocates, though, are loud in their support. The Cancer Support Community says: “No biosimilar-specific safety signals in nine years of monitoring. That’s proof the system works.”What This Means for You
If you’re a patient: You have more options. And those options are cheaper. A biosimilar can save you 15-30% over the original biologic. Ask your doctor if a biosimilar is right for you. Check the FDA Purple Book to see which ones are approved and interchangeable. If you’re a prescriber: You’re not losing control. Biosimilars are not generics. They’re rigorously vetted. The data is there. Don’t let outdated myths hold you back. If you’re a pharmacist: Know the difference between “biosimilar” and “interchangeable.” Only interchangeable products can be substituted without prescriber input - and only if your state allows it. The system isn’t perfect. It’s slow. It’s expensive. But it’s working. And it’s getting better.Are biosimilars the same as generics?
No. Generics are exact chemical copies of small-molecule drugs. Biosimilars are highly similar but not identical copies of complex biologic drugs made from living cells. The approval process for biosimilars is far more complex, requiring extensive analytical, clinical, and immunogenicity testing.
How does the FDA decide if a biosimilar is approved?
The FDA uses a stepwise approach: first, detailed analytical studies to compare molecular structure; then animal studies if needed; followed by human trials to confirm pharmacokinetics and safety; and mandatory immunogenicity testing. The final decision is based on the totality of evidence - all data together must show no clinically meaningful differences in safety, purity, or potency.
What is the FDA Purple Book?
The FDA Purple Book is the official public database of all licensed biologics and their biosimilars. It includes approval dates, interchangeability status, patent information, and exclusivity periods. Updated daily since 2025, it’s the only authoritative source for checking which biosimilars are approved and whether they’re interchangeable.
What does “interchangeable” mean for a biosimilar?
An interchangeable biosimilar has met an extra FDA standard: it can be substituted for the reference product without the prescriber’s permission, and switching between the two won’t increase risk or reduce effectiveness. Only 17 of the 43 approved biosimilars have this status as of 2025.
Why are so few biosimilars actually on the market?
Despite 43 approvals, only 29 have launched. Delays are mostly due to patent litigation by originator companies, payer restrictions, and prescriber hesitation. On average, it takes 11.3 months from FDA approval to market launch, and some take years.
Are biosimilars safe?
Yes. Nine years of post-market surveillance show no biosimilar-specific safety signals. Adverse event rates are statistically identical to reference biologics: 0.8 per 10,000 patients for biosimilars vs. 0.7 for originals, according to the FDA’s Sentinel Initiative.