Vitamin D Analog Selector
Recommended Vitamin D Analogs
Your SelectionsNote: Always consult with your healthcare provider before starting any new vitamin D therapy.
When doctors talk about vitamin D therapy, the conversation often jumps from plain vitamin D3 to a slew of specialized analogs. If you’ve been prescribed Alfacip or are weighing it against other options, you need a clear picture of how each works, who benefits most, and what the trade‑offs are. This guide walks you through the science, the clinical uses, and the practical considerations for Alfacip (alfacalcidol) and its most common alternatives.
What Is Alfacip (Alfacalcidol)?
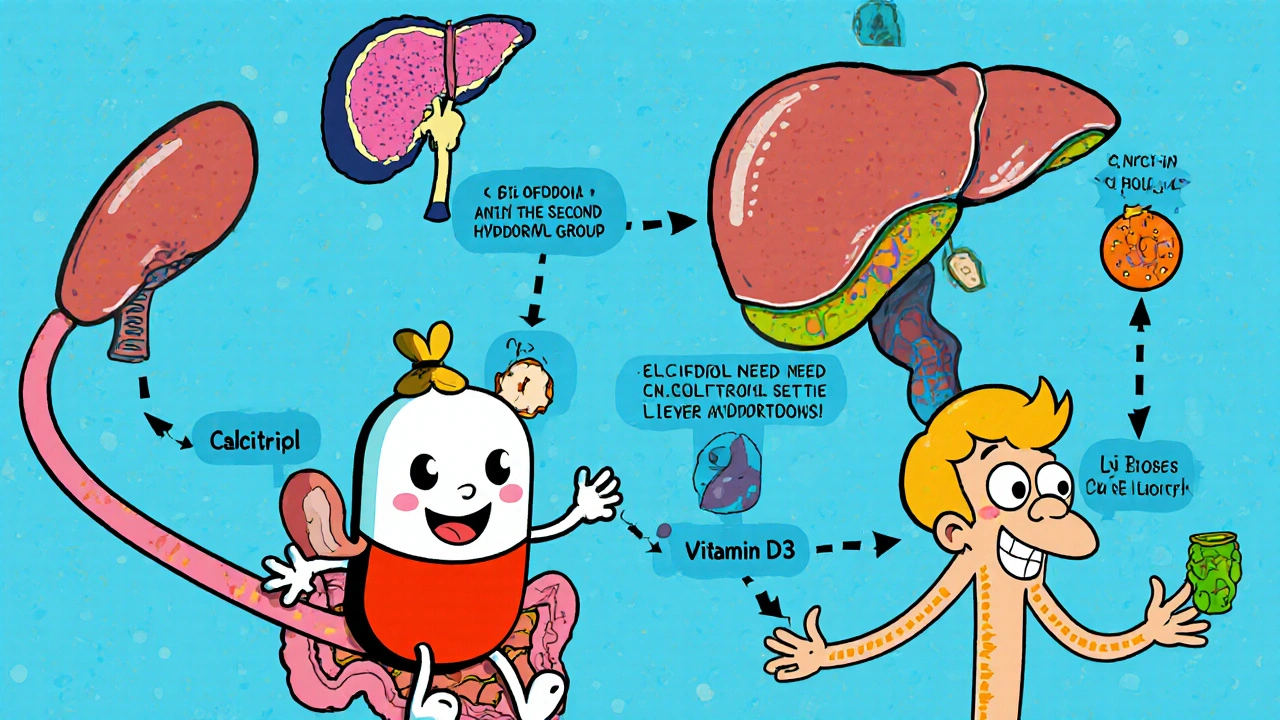
Alfacip is the brand name for alfacalcidol, a synthetic vitamin D analog that belongs to the 1‑hydroxyvitamin D3 family. Unlike natural vitamin D3 (cholecalciferol), alfacalcidol already carries one hydroxyl group, meaning the liver can convert it directly into the active hormone without the first hydroxylation step.
This shortcut is especially useful for patients whose liver function is compromised, such as those with chronic liver disease or certain genetic disorders.
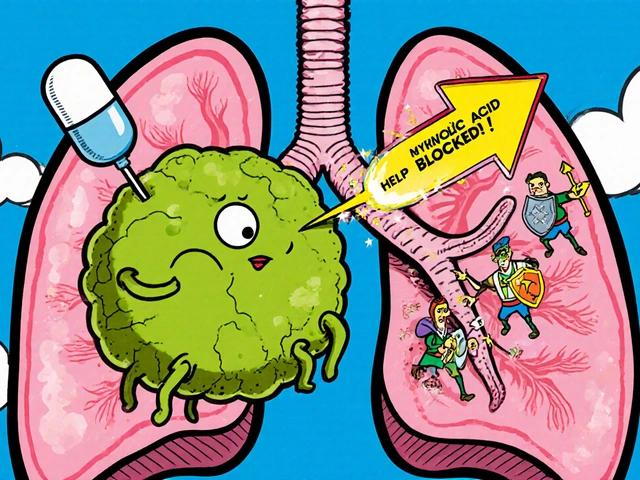
How Alfacip Works in the Body
After oral intake, alfacalcidol is absorbed in the small intestine and enters the bloodstream. The liver quickly adds a second hydroxyl group, converting alfacalcidol into calcitriol, the hormonally active form of vitamin D (1,25‑dihydroxyvitamin D3). Calcitriol then binds to vitamin D receptors (VDR) in target tissues, regulating calcium and phosphate balance, bone remodeling, and immune modulation.
Because the conversion bypasses the initial liver step, alfacalcidol is often preferred for patients with impaired hepatic conversion but normal kidney function.
Key Alternatives to Alfacip
Several other vitamin D analogs and forms are used for similar indications. Below are concise definitions of the most frequently compared compounds.
- Calcifediol (25‑hydroxyvitamin D3) is the product of the first liver hydroxylation of vitamin D3. It requires only renal conversion to become active.
- Calcitriol (1,25‑dihydroxyvitamin D3) is the fully active hormone, usually given in low‑dose prescriptions for severe deficiency or renal osteodystrophy.
- Vitamin D3 (cholecalciferol) is the natural form produced in skin after sun exposure. It undergoes two hydroxylations (liver then kidney) to become active.
- Vitamin D2 (ergocalciferol) is plant‑derived, structurally similar to D3 but generally considered less potent.
Side‑by‑Side Comparison
| Feature | Alfacip (Alfacalcidol) | Calcifediol | Calcitriol | Vitamin D3 (Cholecalciferol) | Vitamin D2 (Ergocalciferol) |
|---|---|---|---|---|---|
| Potency (relative to 1,000 IU D3) | ≈1.5× D3 | ≈3× D3 | ≈10× D3 | Baseline | ≈0.7× D3 |
| Typical oral dose | 0.5-2 µg daily | 20-40 µg (800-1,600 IU) weekly | 0.25-0.5 µg daily | 400-2,000 IU daily | 800-2,000 IU daily |
| Required organ conversion | Liver → active | Liver → kidney → active | Kidney → active (already active) | Liver → kidney → active | Liver → kidney → active |
| Key indications | Renal osteodystrophy, hypoparathyroidism, liver disease | Severe deficiency, malabsorption, chronic kidney disease | Severe hyperparathyroidism, renal osteodystrophy | General deficiency, osteoporosis prevention | General deficiency (when D3 unavailable) |
| Half‑life | ≈20‑30 hours | ≈15‑20 hours | ≈6‑8 hours | ≈15‑20 hours (D3), active form ≈15 hours | ≈15‑20 hours |
| Safety profile | Low risk of hypercalcemia when monitored | Similar to D3, modest hypercalcemia risk | Higher hypercalcemia risk; requires close labs | Very safe at standard doses | Generally safe, slightly less potent |
Factors to Consider When Choosing an Analog
Picking the right vitamin D therapy isn’t a one‑size‑fits‑all decision. Here are the top criteria doctors weigh:
- Organ Function: If liver conversion is impaired, alfacalcidol or calcifediol can bypass that step. For kidney failure, calcitriol may be necessary because it’s already active.
- Severity of Deficiency: Mild to moderate deficiency is often managed with D3 or D2. Severe cases with rapid bone loss may need the higher potency of alfacalcidol or calcitriol.
- Risk of Hypercalcemia: More potent analogs carry a higher calcium‑raising potential. Frequent serum calcium monitoring is mandatory for calcitriol and alfacalcidol.
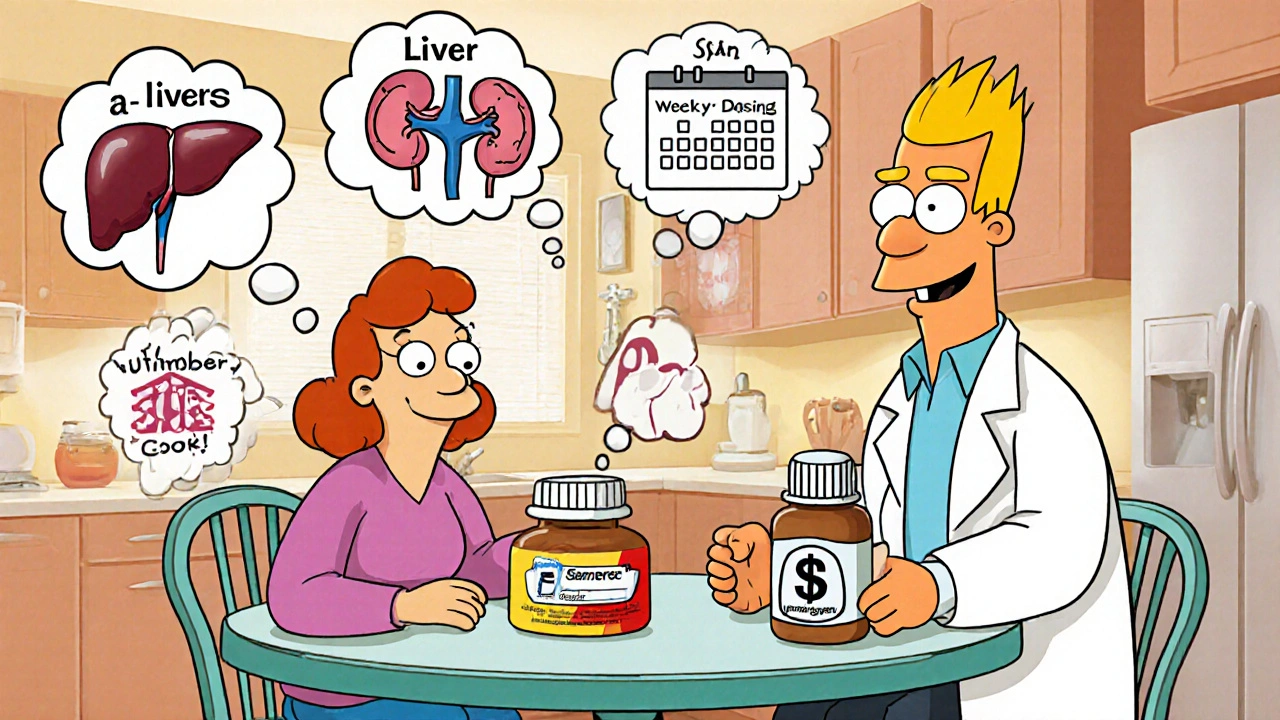
- Convenience & Adherence: Weekly dosing of calcifediol can improve compliance compared to daily pills, especially in elderly patients.
- Cost & Availability: D3 supplements are cheap and widely available. Prescription analogs can be pricier and may require insurance approval.
Practical Dosing & Safety Tips
Regardless of which analog you end up using, the following best practices help keep treatment safe and effective:
- Check baseline serum calcium, phosphate, PTH, and 25‑hydroxyvitamin D levels before starting.
- Re‑test calcium and phosphate after 2‑4 weeks, then every 3 months for the first year.
- Adjust dose gradually; a 25% reduction is typical if calcium rises above the upper normal range.
- Avoid high‑dose over‑the‑counter supplements while on prescription analogs.
- Inform your doctor about thiazide diuretics, lithium, or granulomatous diseases, as these can amplify hypercalcemia risk.
When Alfacip Is the Preferred Choice
Clinical guidelines from the National Institute for Health and Care Excellence (NICE) and KDIGO recommend alfacalcidol for patients with chronic kidney disease stage 3‑5 who have secondary hyperparathyroidism but retain enough kidney function to convert calcifediol. Its moderate potency and liver‑bypass pathway make it a sweet spot for:
- Patients with mild to moderate hepatic impairment.
- Those who need a steady calcium rise without the sharp spikes associated with calcitriol.
- Individuals who have struggled with oral D3 absorption due to fat‑malabsorption syndromes.
Potential Side Effects and Drug Interactions
Common side effects are usually mild but worth monitoring:
- Hypercalcemia (symptoms: nausea, vomiting, weakness, confusion).
- Hyperphosphatemia, especially in renal patients.
- Rare allergic reactions (rash, itching).
Interactions to watch for include:
- Thiazide diuretics: Reduce calcium excretion, raising hypercalcemia risk.
- Anticonvulsants (phenytoin, phenobarbital): Accelerate vitamin D metabolism, potentially lowering efficacy.
- Glucocorticoids: Impair calcium absorption, may require higher doses.
Bottom Line: How to Decide
If you or a loved one are navigating vitamin D therapy, start by asking your healthcare provider these questions:
- Do I have any liver or kidney issues that affect vitamin D metabolism?
- What is my current serum calcium and PTH level?
- Is my bone density at risk for osteoporosis or fractures?
- Can I commit to daily dosing, or would weekly dosing help me stick to the plan?
- What are the cost implications and insurance coverage for each option?
Answering these will guide you toward alfacalcidol, calcifediol, calcitriol, or simple vitamin D3 supplements-and keep you from wasting time and money on the wrong choice.
Frequently Asked Questions
How quickly does Alfacip raise blood calcium levels?
Alfacip typically begins to affect serum calcium within 2‑3 days, reaching a stable plateau after about 2 weeks of consistent dosing.
Can I take Alfacip together with over‑the‑counter vitamin D3?
It’s generally not recommended because the combined effect can push calcium too high. If additional supplementation is needed, your doctor will adjust the alfacalcidol dose instead.
Is Alfacip safe for pregnant women?
Alfacalcidol falls under FDA pregnancy category C; it should only be used if the potential benefit outweighs the risk. Discuss alternatives with your obstetrician.
What monitoring schedule is recommended?
Baseline labs, then repeat calcium, phosphate, and PTH after 2-4 weeks, followed by quarterly checks for the first year. After stability, six‑monthly labs are usually sufficient.
How does Alfacip compare cost‑wise to calcitriol?
In the UK, alfacalcidol (Alfacip) is typically priced around £15‑£20 for a 30‑day supply, whereas calcitriol can run £30‑£45 for the same period, reflecting its higher potency and narrower indication.