Narrow Therapeutic Index Drug Impact Calculator
Understanding Narrow Therapeutic Index (NTI) Drugs
Drugs with a narrow therapeutic index have little room for error. Small changes in dose can lead to ineffective treatment or dangerous side effects. This calculator shows how your individual factors affect the safety margin of NTI medications.
Example: Warfarin requires INR monitoring because a slight overdose could cause bleeding, while too little might lead to dangerous blood clots. Your kidney function, age, and liver health impact how your body processes these critical drugs.
Calculate Your Medication Safety Profile
Your Safety Profile
Risk Level
Therapeutic Index
Why this matters: Your combination of factors shows how much your body processes this medication. This is why regular blood tests (like INR for warfarin) are essential for your safety.
Getting the right dose of medication isn’t just about following the label. It’s about finding the sweet spot where the drug works - without hurting you. Too little, and it does nothing. Too much, and you risk serious side effects - or worse. For many people, especially those on multiple medications or with chronic conditions, this balance is constantly shifting. And it’s not something you should guess at.
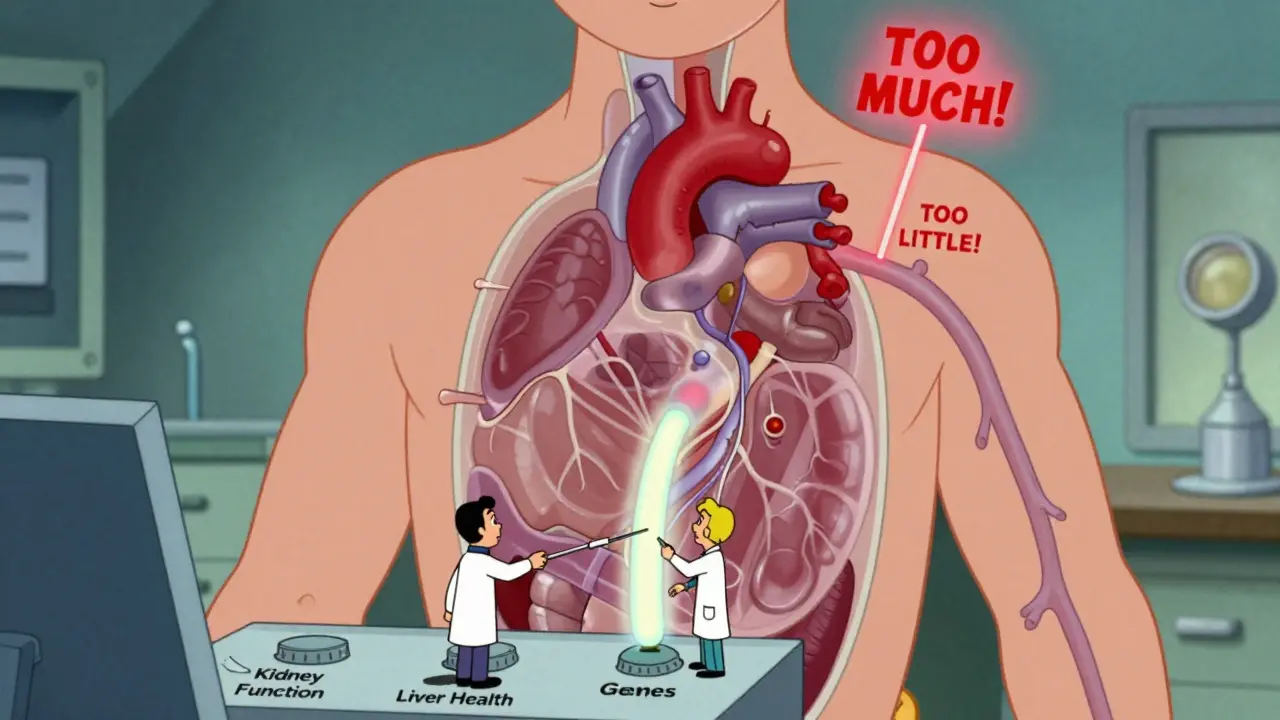
Why One Size Doesn’t Fit All
Your body isn’t the same as your neighbor’s. Age, weight, kidney function, liver health, even your genes can change how a drug moves through you. Take warfarin, a blood thinner. A 70-year-old woman with reduced kidney function might need half the dose of a healthy 40-year-old man. Give her the standard dose, and she could bleed internally. Give him too little, and he could have a stroke. This is why the therapeutic index matters. It’s the ratio between the dose that works and the dose that’s dangerous. Drugs with a narrow therapeutic index (NTI) - like digoxin, phenytoin, or lithium - have almost no room for error. Just a little too much digoxin can stop your heart. Just a little too little, and it won’t help your heart failure. These aren’t drugs you can tweak on your own.Who Needs Close Monitoring?
Not every medication needs careful tuning. Penicillin? You can take a bit more or less without major risk. But for NTI drugs, regular blood tests aren’t optional - they’re lifesaving. Warfarin users need INR checks every 2 to 4 weeks to keep levels between 2.0 and 3.0. Miss a test, and you’re gambling with your life. Older adults are especially vulnerable. About 44% of people over 65 take five or more medications. That’s called polypharmacy. And each extra pill increases the chance of dangerous interactions. A common painkiller like ibuprofen can make warfarin more potent. A simple change in diet - eating more leafy greens - can throw off INR levels. Even a minor infection can slow how your liver breaks down drugs, leading to dangerous buildup.What Factors Change Your Dose?
Your doctor doesn’t just pick a number out of a book. They look at real, measurable things:- Kidney function: Measured by creatinine clearance. If your kidneys aren’t filtering well, drugs like metformin or antibiotics can build up. Doses often drop by 25-50%.
- Liver health: The liver breaks down most drugs. If you have cirrhosis, doses of antidepressants, opioids, or antifungals may need to be cut in half.
- Body weight: For obese patients, dosing isn’t based on total weight. Doctors use ideal body weight plus 40% of excess weight. Giving a 300-pound person the same dose as a 150-pound person can lead to toxicity.
- Age: After 65, metabolism slows. Many drugs require 20-30% lower doses just because of age alone.
- Genetics: About 25% of commonly used drugs are affected by gene variations. For example, some people metabolize codeine too fast - turning it into morphine too quickly - leading to dangerous breathing problems.
The Problem with Clinical Trials
Most drug dosing guidelines come from clinical trials. But here’s the catch: those trials rarely include older adults, pregnant women, or people with three or more chronic diseases. So when your doctor prescribes a dose based on those studies, they’re guessing for you. A 78-year-old with kidney disease, heart failure, and diabetes? She wasn’t in the trial. The label says “take 10 mg daily.” But for her, that could be too much. That’s why real-world experience matters more than trial data for many patients.How Pharmacists Help You Stay Safe
Pharmacists aren’t just the people who hand you pills. They’re the hidden experts in dose adjustment. They know how drugs interact, how food affects absorption, and how to spot when a dose doesn’t fit a patient’s profile. Pharmacist-led clinics for warfarin users have cut major bleeding events by 60%. In nursing homes, pharmacist reviews of medication lists have reduced hospitalizations by 22%. They don’t just check for errors - they ask: “Is this still needed?” Deprescribing - stopping medications that aren’t helping anymore - is just as important as starting them. Many older adults take drugs for conditions that have resolved, or that are now doing more harm than good. A statin for high cholesterol might be fine at 50, but at 80, with no heart disease, the risk of muscle pain or diabetes might outweigh the tiny benefit.What You Can Do
You don’t have to wait for your doctor to bring it up. Here’s how to take control:- Keep a full list: Write down every pill, vitamin, and supplement you take - including doses and times. Bring it to every appointment.
- Ask: “Why am I taking this?” If you don’t know the reason, it might be time to stop.
- Ask about alternatives: Is there a drug with a wider safety margin? Could a lower dose work?
- Know your warning signs: For digoxin: nausea, blurred vision, irregular heartbeat. For lithium: tremors, confusion, frequent urination. Report them immediately.
- Don’t skip blood tests: If your doctor says you need an INR or drug level check, don’t cancel it. That test is your safety net.
The Future: Dosing That Fits You
The future of medication isn’t one-size-fits-all. It’s one-dose-fits-one-person. Companies like DoseMe and InsightRX are using AI to predict the right dose by combining your genetics, weight, kidney function, and even your diet. The FDA is pushing for this too - new drugs will soon need to show how dosing changes across different patient groups. In the next five years, we’ll see more clinics using real-time data to adjust doses. Imagine a wearable that tracks your heart rhythm and sends alerts if your digoxin level is creeping up. Or a smartphone app that tells you, based on your last lab results, whether your warfarin dose needs a tweak. But for now, the best tool you have is awareness. Know your meds. Know your body. Speak up when something feels off. The right dose isn’t written on a prescription pad - it’s found through careful observation, testing, and honest conversations with your care team.When to Call Your Doctor
You don’t need to wait for your next appointment. Call right away if you notice:- New dizziness, confusion, or fainting
- Unusual bleeding or bruising
- Severe nausea, vomiting, or diarrhea
- Changes in heart rate or rhythm
- Swelling in your feet or hands
- Any new symptom that started after a dose change
What if I miss a dose of my medication?
Don’t double up unless your doctor says so. For most drugs, if you miss a dose by a few hours, take it as soon as you remember. If it’s almost time for the next dose, skip the missed one. But for NTI drugs like warfarin or digoxin, always call your provider - the timing matters more than you think. Some drugs require exact intervals to stay safe.
Can I adjust my dose myself if I feel better or worse?
No. Even if you feel better, stopping or lowering your dose without medical advice can be dangerous. For example, stopping an anticonvulsant suddenly can trigger seizures. Feeling worse doesn’t always mean you need more - it could mean you’re getting too much. Only your doctor or pharmacist can safely interpret how you’re responding.
Are generic drugs the same dose as brand-name ones?
For most drugs, yes - generics must meet strict standards to be approved. But for NTI drugs like levothyroxine or phenytoin, even small differences in absorption can matter. If you switch brands, your doctor may want to check your blood levels again. Stick with the same generic brand if possible, and always tell your pharmacist if you notice a change in how you feel.
How long does it take for a dose change to work?
It depends on the drug. Some, like antibiotics, show effects in days. Others, like antidepressants or blood pressure meds, take weeks. For NTI drugs, it’s not just about when you feel better - it’s about when the drug levels stabilize in your blood. That’s why follow-up tests are scheduled weeks after a change. Patience is part of the process.
Do I need to tell my pharmacist about supplements and herbs?
Absolutely. St. John’s wort can cut the effectiveness of birth control, antidepressants, and even some cancer drugs. Garlic and ginkgo can thin your blood like aspirin. Grapefruit juice can make cholesterol drugs dangerously strong. Your pharmacist needs to know everything you’re taking - not just prescriptions.