For years, if your GP prescribed a branded drug like Amoxil, your pharmacist could swap it for a cheaper generic version of amoxicillin - unless your doctor specifically said ‘dispense as written’. That’s changing. As of October 1, 2025, the rules around what medicines you get, and how you get them, have been rewritten. The NHS is no longer just swapping pills. It’s swapping entire care models.
What’s Really Changing with Generic Medicines?
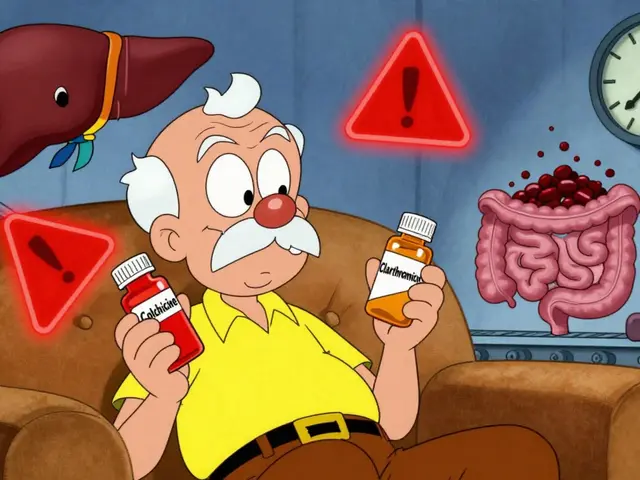
The old rule was simple: pharmacists could substitute branded drugs with generics unless the prescription said otherwise. That’s still true, but now there’s a new target: 90% of eligible prescriptions must be filled with generics. That’s up from 83% in early 2025. The goal? Save money without hurting outcomes. And it’s working - generic medicines cost up to 80% less than branded ones, and studies show they work just as well for most conditions. But here’s the catch: not all patients are the same. Elderly patients on multiple meds, people with mental health conditions, or those with complex allergies need more care. The 2025 reforms don’t change the substitution rule itself, but they do tighten how it’s enforced. Pharmacists now have to log every substitution in a central digital system. If a patient gets switched three times in six months, the system flags it for review. It’s not about stopping substitutions - it’s about making sure they’re safe.Pharmacy Doors Are Closing - Literally
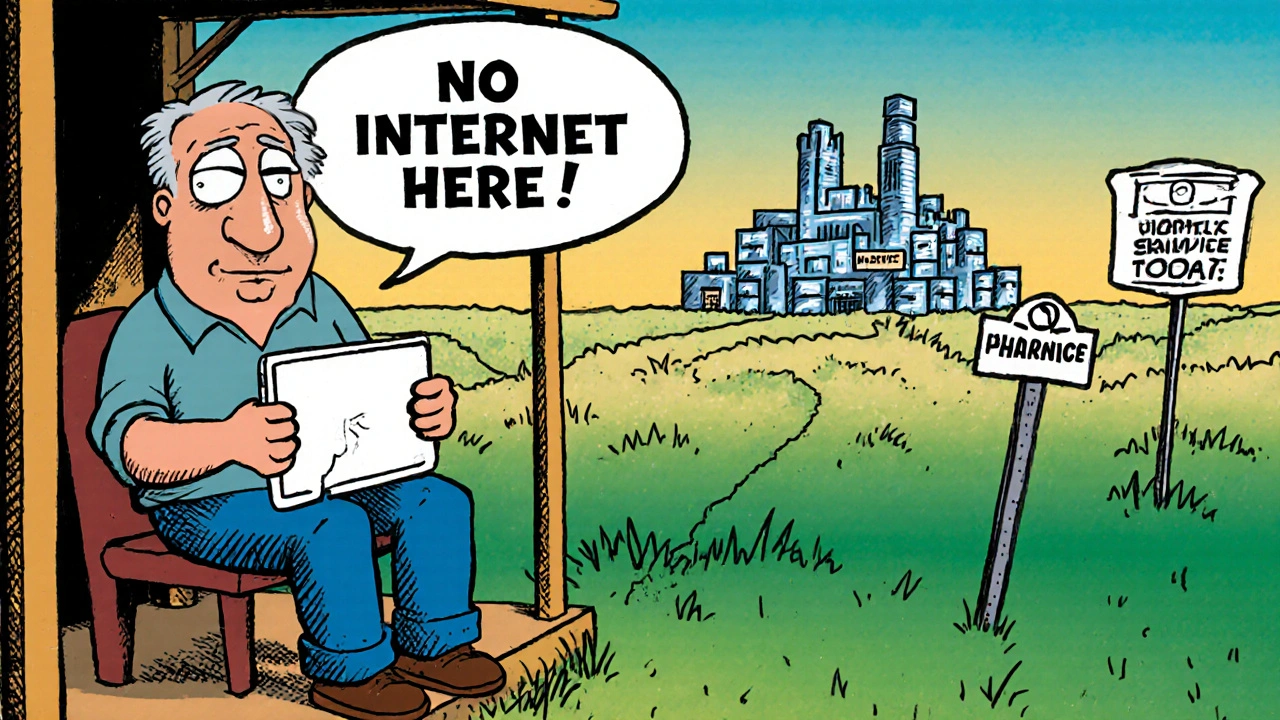
The biggest shock? You won’t need to walk into a pharmacy anymore to get your meds. Starting October 2025, all NHS pharmaceutical services must be delivered remotely by Digital Service Providers (DSPs). That means no more in-person consultations, no more face-to-face advice from your pharmacist, and no more picking up your prescription from the counter. Instead, your prescription goes digital. A DSP - often a large company with a warehouse and a call center - processes it, packages your meds, and sends them by courier. You’ll get a text or email with tracking info. If you have questions, you call a hotline. There’s no pharmacist on-site anymore. This isn’t just a convenience shift. It’s a legal change. The Human Medicines (Amendment) Regulations 2025 removed the requirement for pharmacies to have a physical premises to qualify for NHS contracts. New providers can now enter the market without opening a shop. Existing pharmacies can still operate, but only if they meet the new DSP standards - which means spending between £75,000 and £120,000 on digital systems, delivery logistics, and remote support tools. Many community pharmacies say they can’t afford it. In the North West, 54% of pharmacies surveyed said they’d have to shut down if forced to comply. Others are merging into larger networks just to survive.Service Substitution: From Hospital to Home
It’s not just about pills. The NHS is moving care out of hospitals and into your living room, your GP’s office, or a local community hub. The 2025 mandate says it clearly: “Move care from hospital to community, sickness to prevention, analogue to digital.” That means:- Virtual fracture clinics replacing in-person follow-ups
- Community diagnostic hubs taking over X-rays and blood tests once done in hospitals
- Remote monitoring for heart failure or COPD using smart devices sent to your home
- Home visits by nurses instead of emergency department trips
Who’s Getting Left Behind?
The data is clear: substitution is widening gaps. A King’s Fund report from June 2025 found that in deprived areas, care access got worse after substitution programs rolled out. Why? Because the system assumed everyone had digital access, transport, or family support. They didn’t. - A 78-year-old woman in Hull couldn’t use her virtual diabetes appointment because her tablet was broken and she couldn’t afford a new one. She missed her check-up and ended up in A&E with a foot infection. - A man in rural Cumbria had his joint replacement follow-up moved to a community hub 20 miles away. He doesn’t drive. No bus runs on Sundays. He skipped it. His pain got worse. - In London, a patient with dementia had his meds delivered remotely. His caregiver didn’t know how to read the digital instructions. He took double the dose. These aren’t rare cases. The British Medical Association reports a 12% spike in medication errors in areas with remote dispensing. Nurses are seeing more patients with preventable complications - not because the care was bad, but because the system didn’t account for real life.The Workforce Gap
The NHS wants to shift care to the community. But who’s going to do it? Right now, there’s a shortage of 28,000 community health workers - nurses, physiotherapists, social care assistants - needed to make this work. In 68% of Integrated Care Boards, staff say they’re already stretched too thin. In rural areas, 42% of trusts don’t even have the basic infrastructure to deliver home visits or community clinics. The government’s solution? Train more people. But training a community nurse takes three years. The 10-Year Health Plan says they need 15,000 more by 2030. That’s not a plan - it’s a wish. Meanwhile, hospital pharmacists - the ones who used to check your meds face-to-face - are being moved into remote roles. Many are leaving. The NHS Staff Survey 2025 showed 78% of hospital pharmacists are worried about safety in the new system. They’re not against change. They’re against being forced to do more with less, and no backup.
What This Means for You
If you’re on long-term meds, here’s what to expect:- Your prescription will likely be filled with a generic version - unless your doctor says no.
- You’ll get your meds by post or courier, not from a local pharmacy.
- You may be asked to use a phone app or online portal to manage your care.
- If you can’t use tech, you need to tell your GP now. There’s still a right to face-to-face support - but you have to ask for it.
What’s Next?
The next big change? The Carr-Hill formula update in April 2026. It will shift funding to areas with the worst health and economic challenges. That could mean more investment in deprived towns - or more pressure on already struggling services. By 2030, the NHS wants 45% of outpatient appointments to be virtual or community-based. That’s 10 million appointments moved. If done right, it could cut waiting lists by 35%. If done poorly? It could cost the NHS more in the long run - through avoidable hospital admissions, medication errors, and lost trust. The real question isn’t whether substitution works. It’s: who gets to decide what’s safe? And who’s left out when the system moves on?Can my pharmacist still give me the branded medicine if I want it?
Yes - but only if your doctor writes ‘dispense as written’ (DAW) on the prescription. Otherwise, the NHS requires pharmacists to offer the cheapest generic equivalent. You can ask for the branded version, but you may have to pay the price difference out of pocket if it’s not covered by NHS rules.
Do I have to use digital services for my NHS care now?
No. The law still allows for face-to-face care if you need it. But the system is being redesigned to push people toward digital and remote options. If you can’t use apps, phones, or online portals, you must tell your GP or practice nurse. They’re legally required to offer alternatives - but you need to speak up. Don’t wait until you’re left behind.
Why are pharmacies closing or changing how they work?
Because the 2025 NHS reforms require all NHS pharmaceutical services to be delivered remotely by Digital Service Providers. Many small pharmacies can’t afford the £75,000-£120,000 in tech upgrades needed. Some are shutting down. Others are joining larger networks that can handle the cost. It’s not about choice - it’s about survival under new rules.
Will I still be able to get my meds if I live in a rural area?
It depends. In areas with poor internet or no courier access, the NHS is supposed to provide alternative delivery methods - like mobile clinics or local partnerships. But many rural areas don’t have the infrastructure yet. If you’re worried, contact your local Integrated Care Board. Ask what support is available. Don’t assume it’s there - ask for it.
Are generic medicines safe?
Yes. Generic medicines must meet the same strict safety and quality standards as branded drugs. They contain the same active ingredient, in the same dose, and work the same way. The only differences are in inactive ingredients (like fillers) or packaging - which don’t affect how the medicine works. Most patients switch without any issues.
What should I do if I think my substitution caused a problem?
Contact your GP or pharmacist immediately. If you’ve had a bad reaction, side effect, or missed care because of a substitution, report it. You can also file a formal complaint with your local Integrated Care Board. Keep records of your prescriptions, dates, and symptoms. The NHS tracks substitution errors - but only if you tell them.