Medication Hiccup Risk Calculator
Check Your Medication Risk
Select medications you're currently taking to see your risk of medication-induced hiccups.
Most people think hiccups are just a silly, harmless annoyance-something you get after eating too fast or drinking soda too quickly. But when hiccups stick around for days, or even weeks, they’re not funny anymore. They keep you from sleeping, eating, or even talking without interruption. And for many, the cause isn’t a big meal or a laugh too hard-it’s a medication they’re taking.
Why Your Medicine Might Be Making You Hiccup
Hiccups happen when the diaphragm, the muscle under your lungs, spasms suddenly. That spasm pulls air in fast, and your vocal cords snap shut, making the classic "hic" sound. It’s a reflex controlled by nerves in your brainstem. But certain drugs can mess with that reflex. They don’t just cause nausea or drowsiness-they can trigger this strange, stubborn reaction. The most common offenders are corticosteroids, especially dexamethasone. It’s often given to cancer patients before chemotherapy to reduce nausea and swelling. But in up to 41% of patients on high doses, it triggers hiccups. One person on Reddit described getting 8mg of dexamethasone and then being hiccups for 72 hours straight. That’s not rare. In fact, the FDA added hiccups to the official side effect list for dexamethasone in 2021 because so many reports came in. Other drugs linked to hiccups include:- Opioids like morphine and oxycodone-especially in chronic pain patients. About 5-7% report hiccups, likely because the drugs slow digestion and cause stomach bloating.
- Benzodiazepines like midazolam, often used before surgery. Around 10% of patients hiccup after receiving them.
- Cisplatin, a chemotherapy drug. When paired with dexamethasone, the hiccup risk jumps dramatically.
- Antibiotics like azithromycin or moxifloxacin-rare, but documented. One case in 2023 involved a man who developed hiccups after starting moxifloxacin for tuberculosis.
It’s not always about the dose. Even low amounts of dexamethasone-like 4mg daily-can trigger hiccups in sensitive people. And because hiccups aren’t usually listed as a top side effect on drug labels, doctors often miss the connection. A 2019 study found that 35% of medication-induced hiccup cases were misdiagnosed as something else.
What Happens in Your Body When a Drug Causes Hiccups
It’s not just "the drug makes you hiccup." There’s a real biological reason. Some drugs directly irritate the vagus or phrenic nerves-those are the wires running from your brain to your diaphragm. Others affect brain chemicals like dopamine or GABA, which help control reflexes. Dexamethasone, for example, may activate steroid receptors near the hiccup center in your brainstem. Opioids, on the other hand, slow down your gut. That leads to gas buildup and stomach pressure, which tugs on the diaphragm. That’s why people on long-term pain meds often hiccup after eating. It’s not the drug itself-it’s the side effect it creates in your belly. The good news? Once you know the cause, you can often fix it without a ton of testing. No need for CT scans or endoscopies if the hiccup started right after you began a new drug.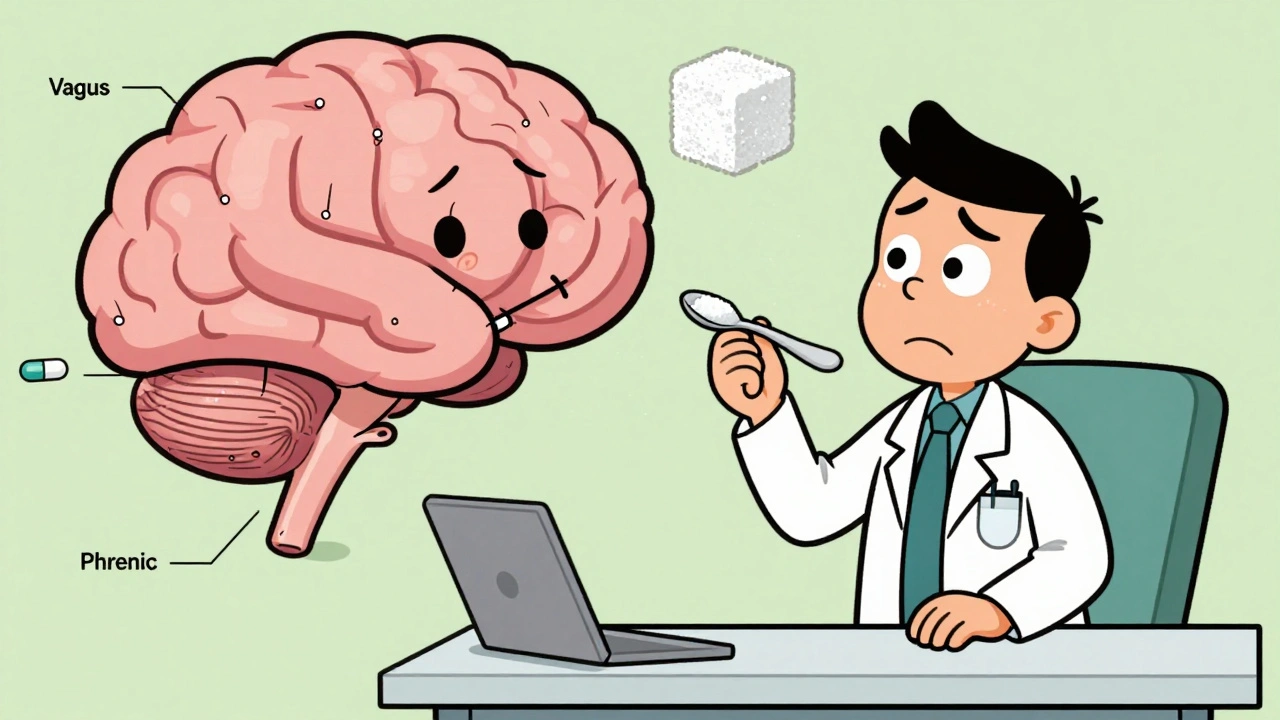
What to Do When Hiccups Won’t Stop
If you’ve had hiccups for more than 48 hours, it’s time to take action. Don’t just wait it out. Here’s what works, based on real clinical data:- Check your meds. Look at everything you started in the last week. Did you begin dexamethasone? A new painkiller? Antibiotics? Talk to your doctor about timing.
- Try simple home tricks. Swallowing a teaspoon of granulated sugar has a 72% success rate in stopping hiccups, according to a 2021 JAMA study. Gargling ice water works 65% of the time. Holding your breath for 10-20 seconds can also reset the nerve reflex.
- Don’t stop your medicine without talking to your doctor. If you’re on dexamethasone for cancer treatment, stopping it isn’t safe. But your doctor can switch you to another steroid like prednisone, or add a drug to block the hiccups.
For persistent cases, doctors often prescribe:
- Baclofen (5mg, 3 times a day)-a muscle relaxant that targets GABA receptors. It works in 60-70% of steroid-induced hiccup cases.
- Chlorpromazine (25-50mg daily)-the only FDA-approved drug for hiccups. But it can cause drowsiness, low blood pressure, or movement issues, so it’s not first choice unless other options fail.
- Ondansetron (Zofran)-a nausea drug that’s surprisingly effective for hiccups too. One patient reported hiccups vanished within two hours after switching from dexamethasone to ondansetron.
Some patients even get relief with acupuncture or nerve blocks, but those are last-resort options. The goal is always to treat the cause, not just the symptom.
When You Can’t Stop the Medicine
This is the hardest part. Many people-especially those with cancer-can’t stop taking the drug that’s causing hiccups. Dexamethasone is often essential to make chemotherapy tolerable. So what then? The answer is prevention. A 2012 study in Taiwan showed that giving cancer patients 5mg of baclofen twice daily before their dexamethasone dose cut hiccup rates from 41% down to just 13%. That’s a huge win. Now, many oncology centers in the U.S. and Europe use this protocol routinely. The American Society of Clinical Oncology now recommends screening for hiccups in all patients starting dexamethasone. They’ve even created a simple scoring system called the Hiccup Symptom Score (HSS) to track severity. In 2019, only 12% of cancer centers used it. By 2023, that number jumped to 67%.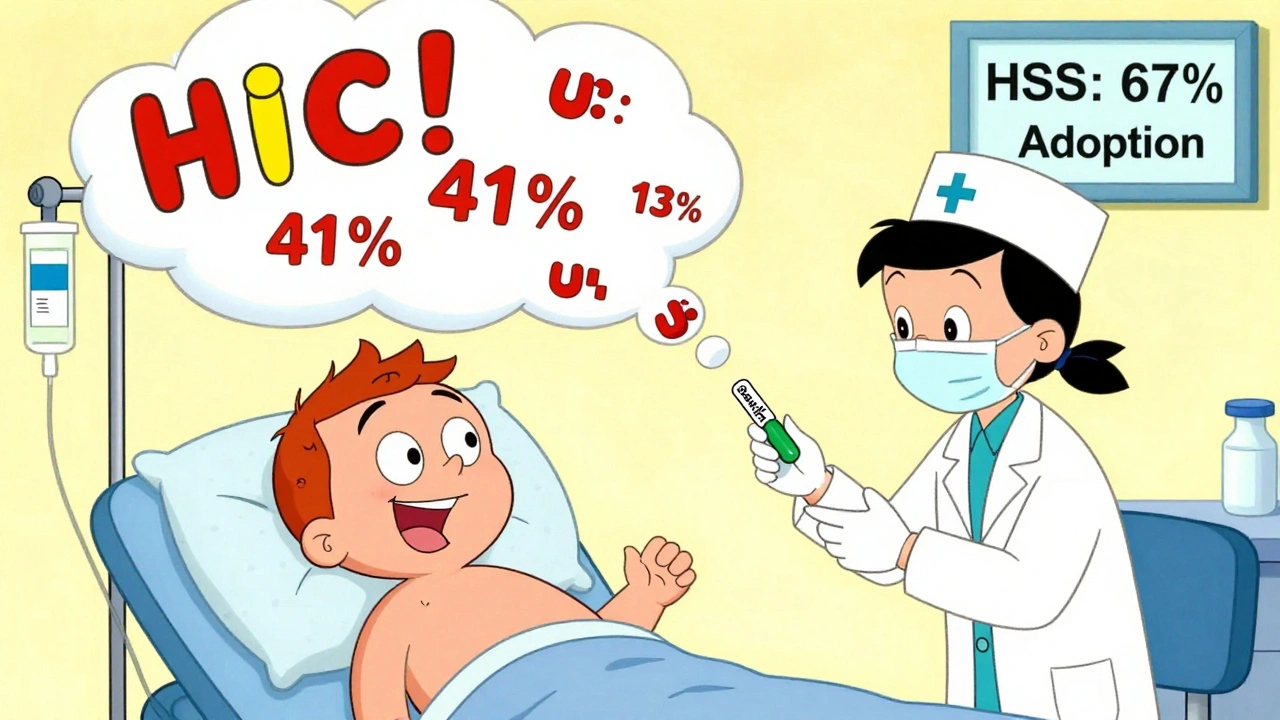
Why This Matters More Than You Think
Hiccups might seem small, but they’re not. Persistent hiccups can lead to weight loss, exhaustion, depression, and even cracked ribs from constant spasms. A 2022 study estimated that proper management of medication-induced hiccups could save the U.S. healthcare system nearly $29 million a year by cutting down on unnecessary tests and ER visits. And it’s getting more attention. In January 2024, the American Medical Association created a new ICD-10 code specifically for medication-induced hiccups: R09.2-MIH. That means doctors can now officially document it-and insurance companies can’t ignore it. Even the FDA is responding. They’ve started requiring hiccup data in clinical trials for all new drugs that affect the nervous system or stomach. That’s a big shift. Five years ago, this was rarely tracked. Now, it’s standard.What You Should Do Right Now
If you’re hiccuping and on a new medication:- Write down when the hiccups started and what drugs you began around that time.
- Try sugar or ice water. If it helps, it’s likely drug-related.
- Call your doctor. Don’t wait. Say: "I started [drug name] and now I can’t stop hiccuping. Could this be related?"
- If you’re on dexamethasone or opioids, ask about baclofen as a preventive option.
Most cases resolve once the drug is adjusted or stopped. But if you ignore it, you risk months of discomfort-and possibly more serious health problems.
Medications save lives. But they can also cause strange, overlooked side effects. Hiccups are one of them. The good news? You don’t have to suffer through it. With the right knowledge, you can get relief-and get back to living without that annoying "hic" every few seconds.
Can any medication cause hiccups?
Not all medications cause hiccups, but some are far more likely. The top culprits are corticosteroids like dexamethasone, opioids like morphine, benzodiazepines like midazolam, and certain chemotherapy drugs like cisplatin. Antibiotics and other drugs can trigger hiccups too, but it’s rare. The key is timing-if hiccups started within a few days of beginning a new drug, that drug is the likely cause.
How long do medication-induced hiccups last?
Most last less than 48 hours and go away on their own. But in about 30% of cases, they become persistent-lasting more than 48 hours. A small number (around 5%) turn into intractable hiccups, lasting over a month. The longer they last, the more likely they’re tied to a medication that needs to be adjusted or treated with another drug.
Is there a cure for drug-induced hiccups?
There’s no single "cure," but there are proven solutions. Stopping or switching the drug often works. If you can’t stop it, baclofen or chlorpromazine are the most effective medications. Simple remedies like sugar or ice water help many people. In cancer patients, giving baclofen before dexamethasone reduces hiccup rates by more than 70%.
Why don’t doctors always know about this side effect?
Because it’s not listed as a top side effect on most drug labels. Hiccups are often buried in small print or left out entirely. Many doctors aren’t trained to connect hiccups with medications unless they’ve seen it before. A 2023 FDA survey found only 37% of providers correctly identified medication-induced hiccups. That’s changing, but awareness is still low.
Can I treat medication-induced hiccups at home?
Yes, for mild or recent cases. Try swallowing a teaspoon of sugar, gargling ice water, or holding your breath for 10-20 seconds. These methods work in over half of cases. But if hiccups last more than two days, or if you’re on a serious medication like chemotherapy drugs, don’t rely on home remedies alone. Talk to your doctor-you may need a prescription to stop them for good.
Are there any new treatments for medication-induced hiccups?
Yes. In June 2023, the FDA gave breakthrough status to a new drug called GBX-204, a GABA-B receptor agonist that’s showing 82% effectiveness in clinical trials-better than baclofen. It’s not available yet, but it’s expected to be approved by 2026. Meanwhile, the new ICD-10 code R09.2-MIH, introduced in January 2024, helps doctors track and treat these cases more accurately.