Global Drug Approval Comparison Tool
This tool helps you understand how different regulatory agencies approach drug approval based on key factors like disease severity, available data, and benefit-risk assessment.
Drug Approval Parameters
Adjust the sliders to see how different factors affect approval decisions in each region.
Approval Simulation Results
Every pill you take, every injection you get, every inhaler you use - it didn’t just appear on a pharmacy shelf. It passed through a complex, often conflicting, system of rules designed to keep you safe. But those rules aren’t the same everywhere. In the United States, the FDA decides. In Europe, it’s a mix of Brussels and national agencies. In Canada, Australia, and beyond, different agencies with different priorities make their own calls. And when a drug is approved in one country but flagged as risky in another, patients don’t always know why - or what to do.
How the U.S. FDA Works: Centralized, Fast, But Rigid
The U.S. Food and Drug Administration (FDA) runs a single, centralized system. One agency. One approval process. That means consistency. If the FDA says a drug is safe, it’s safe across all 50 states. No confusion. No patchwork of state-level rules.That structure lets the FDA move quickly on breakthrough treatments. In 2022, the average approval time for a new drug was just over 10 months. For cancer drugs and rare disease therapies, the FDA often fast-tracks approval based on smaller, faster trials. That’s why the U.S. approved 18.3% more rare disease drugs than the EU in 2022.
But there’s a trade-off. The FDA’s process is predictable - but inflexible. When a safety issue pops up, the agency has to go through its own internal review before issuing a warning. During the pandemic, review times jumped by 37% because the system wasn’t built to handle sudden, massive surges in applications.
Doctors in the U.S. report high satisfaction with FDA communications. Eighty-three percent say safety alerts are timely and actionable. But behind the scenes, the paperwork is brutal. A single new drug application can run 15,000 to 20,000 pages. Companies spend millions just to get it right.
The EU’s Hybrid System: More Layers, More Flexibility
The European Union doesn’t have one regulator. It has a network. The European Medicines Agency (EMA) handles new, complex medicines - like biologics and gene therapies - through a centralized process. But for generics and older drugs, each country’s own agency (like Germany’s BfArM or France’s ANSM) makes the call.This creates flexibility. If a country sees a new safety signal, it can act fast - and other EU nations often follow. When the painkiller Vioxx was pulled from the market, 22 EU countries coordinated their response in just 14 days. In the U.S., it took 28.
But that flexibility comes at a cost. For pharmaceutical companies, navigating 27 different national rules for some drugs is a nightmare. Two-thirds of EU-based drugmakers say the system is too complex. Approval times for centralized drugs average 12.7 months - slower than the FDA’s.
On the plus side, EMA’s benefit-risk reports are considered more detailed and easier to understand. Seventy-one percent of European doctors rate them as comprehensive. The EU also approved 12.7% more cancer drugs than the FDA in 2022, because its risk-benefit thresholds are slightly looser. It’s willing to approve drugs with more uncertainty - if the need is high enough.
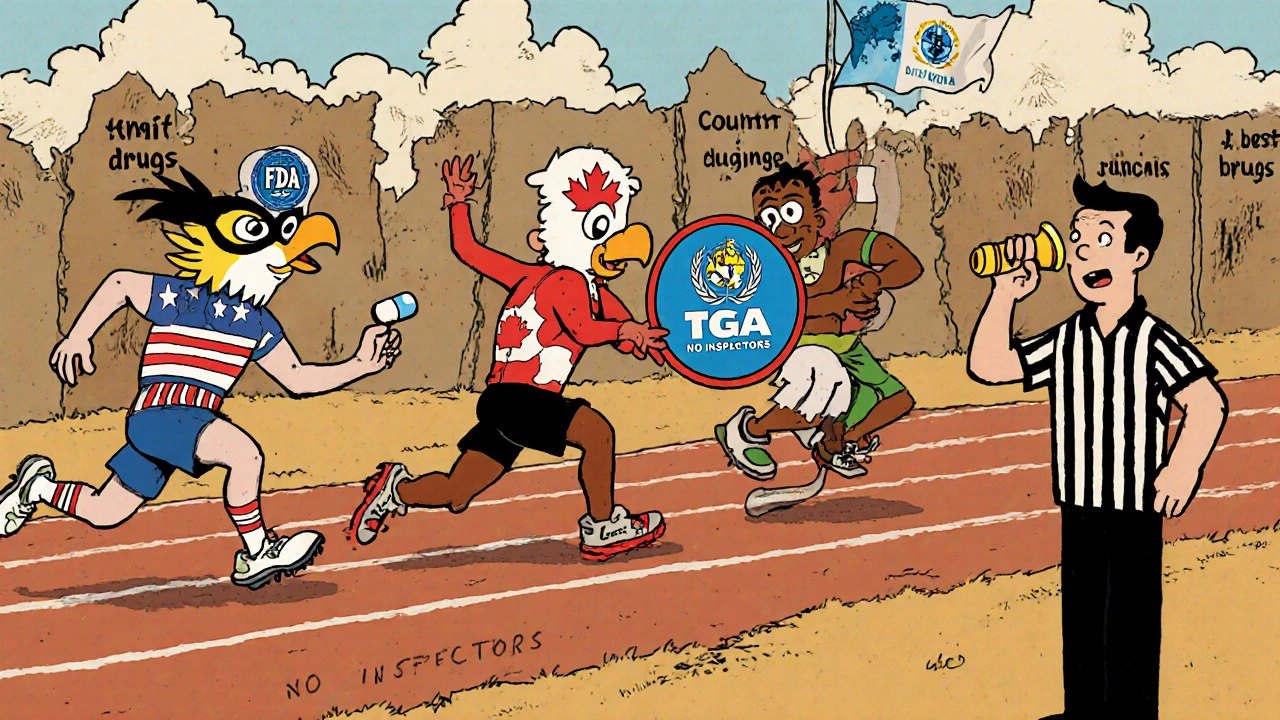
Canada and Australia: Middle Ground with Global Ties
Canada’s Health Canada and Australia’s Therapeutic Goods Administration (TGA) sit between the U.S. and EU models. They’re independent, but they’ve built strong ties with both.Canada signed a Mutual Recognition Agreement (MRA) with the EU in 2019. That means if a drug passes GMP inspections in the EU, Canada accepts it - no repeat inspections. The result? 87% alignment with EU safety decisions. Australia’s TGA does the same with the FDA - 79% concordance on safety alerts.
But neither country fully mirrors either system. Australia’s TGA is known for being cautious. It often waits for more data before approving new drugs, especially biologics. Canada leans toward speed, but still requires local clinical trial data for many drugs. Both have fewer resources than the FDA or EMA, so they rely heavily on international reviews to save time.
That’s why the TGA and Health Canada are often called “reference regulators.” They watch what the FDA and EMA do - and then decide whether to follow, delay, or reject. It’s smart. It’s efficient. But it also means patients in these countries may get new drugs later than those in the U.S. or EU.

The WHO’s Role: Guidelines, Not Laws
The World Health Organization (WHO) doesn’t approve drugs. It doesn’t inspect factories. It doesn’t issue recalls. But its guidelines shape how over 150 countries - especially low- and middle-income ones - regulate medicines.WHO’s Good Manufacturing Practices (GMP) are the global baseline. They’re not legally binding, but they’re the standard everyone points to. When India, Nigeria, or Kenya update their drug laws, they often copy WHO’s language. The WHO’s 2023 Global Benchmarking Tool now rates national regulators on 89 indicators. By the end of 2022, 67 countries reached “Maturity Level 3” - meaning they have a functional, if not perfect, system.
The problem? Many of these countries lack the inspectors, labs, and funding to enforce those standards. In Africa, only 37% of drug manufacturing facilities meet even basic GMP requirements. In places like Bangladesh and Nigeria, patients sometimes get counterfeit or substandard drugs because local regulators can’t check them.
That’s why the WHO’s real power isn’t in enforcement - it’s in setting the conversation. When the WHO flags a drug as unsafe, it’s often the first signal that something’s wrong. But without local action, that warning doesn’t reach the patient.
Why Safety Warnings Don’t Match Up
Here’s one of the most alarming facts: only 10.3% of safety warnings issued by the U.S., Canada, the U.K., and Australia are the same.That means a drug considered safe in one country could be pulled in another - for the exact same side effect. Why? Because regulators weigh risk differently.
The FDA might say: “The benefit outweighs the risk for this group of patients.” The EMA might say: “We need more data before we allow this use.” Australia might say: “We’ll restrict it to hospitals only.”
It’s not about who’s right or wrong. It’s about culture, resources, and legal frameworks. The FDA prioritizes speed and access. The EMA prioritizes transparency and caution. Canada and Australia try to balance both.
Doctors and patients are left guessing. A patient taking a drug in Germany might hear a warning. The same patient in the U.S. gets no notice. That’s not just confusing - it’s dangerous. As former CDC Director Dr. Thomas Frieden put it, this fragmentation puts patients at risk when medications cross borders.
The Cost of Compliance: Millions, Not Minutes
Making a drug safe isn’t just about science. It’s about paperwork, inspections, and legal hoops.A single company trying to sell a drug in the U.S., EU, Canada, and Australia spends an average of $1.2 million just to set up its global regulatory team. It takes 18 to 24 months to train staff to handle all the rules.
And the documentation? It’s insane. FDA submissions average 15,000-20,000 pages. EMA submissions are slightly shorter, but still 12,000-18,000 pages. That’s not a report - it’s a library.
That’s why smaller companies struggle. They can’t afford to file in all markets. So they pick one - usually the U.S. or EU - and wait. That delays access for patients in other countries.
Even the International Council for Harmonisation (ICH) - the group trying to align global rules - admits progress is slow. Their E6(R3) guidelines cut clinical trial paperwork by 22%, but only 89% of major regulators adopted them. The rest? Still using old systems.
What’s Changing? AI, Digital Tools, and the Push for Harmony
The good news? Things are starting to shift.The FDA is using AI to review manufacturing inspections. In 2022, AI handled 43% of routine checks. That’s freeing up inspectors for high-risk sites. The EMA’s Innovation Task Force reviewed nearly 200 advanced therapies last year - many using digital tools to speed up reviews.
The FDA’s 2022 Modernization Act 2.0 removed mandatory animal testing for some drugs - a move that could cut approval times by up to six months. The EU’s Pharmaceutical Strategy aims to cut approval times by 25% by 2025.
And the ICH is pushing for 75% alignment of major rules across the U.S., EU, Japan, and Canada by 2028. That’s ambitious. But it’s also necessary.
Because here’s the truth: no single country can solve global medication safety alone. A drug made in India, tested in Brazil, approved in the U.S., and taken by a patient in Germany - that’s the new reality. If regulators don’t talk to each other, patients pay the price.
What This Means for You
You don’t need to know the difference between EMA and FDA. But you should know this: the drug you take might have been approved under different rules than the one your neighbor takes. And if you travel, or get medication shipped from abroad, you might be taking something that’s not approved - or even flagged as risky - in your home country.Always check your country’s health authority website for safety alerts. Don’t assume a drug is safe just because it’s sold online or in another country. If you’re on multiple medications, talk to your pharmacist. Ask: “Has this drug been flagged anywhere else?”
Global medication safety isn’t just about science. It’s about communication, transparency, and trust. Right now, we’re still building that system - one country, one regulation, one warning at a time.
Why do some drugs get approved in the U.S. but not in Europe?
The FDA often approves drugs faster based on smaller clinical trials, especially for serious or rare diseases. The EMA tends to require more data on long-term safety and broader patient use before granting approval. For example, the FDA approved more rare disease therapies in 2022 because its risk-benefit threshold is lower for conditions with few treatment options. The EMA, by contrast, often waits for stronger evidence of benefit - even if that means slower access.
Is a drug from Canada safer than one from the U.S.?
Not necessarily. Canada’s Health Canada uses the same quality standards as the U.S. and EU for manufacturing. The main difference is in how quickly they approve new drugs. Canada often waits for U.S. or EU decisions before acting, so drugs may arrive later - but they’re still held to the same safety and purity standards. If a drug is approved in Canada, it meets strict GMP and efficacy requirements.
Can I trust drugs from developing countries?
It depends. Many countries in Asia, Africa, and Latin America have strong regulatory agencies that follow WHO guidelines. But enforcement varies. In places with weak inspection systems, counterfeit or substandard drugs are a real risk. If you’re buying medication from abroad, stick to licensed pharmacies and avoid unregulated online sellers. Look for WHO prequalification or local regulatory approval on the packaging.
Why don’t all countries use the same drug approval system?
Each country has different priorities, legal systems, and resources. The U.S. values speed and innovation. The EU values transparency and national input. Canada and Australia prioritize efficiency by using international reviews. Low-income countries often lack funding for full regulatory infrastructure. Harmonization efforts like the ICH are helping, but political, cultural, and economic differences make full global alignment unlikely anytime soon.
How do I know if my medication has been recalled in another country?
Check your country’s health agency website - like the FDA, EMA, or Health Canada. Some countries publish alerts in English. You can also search the WHO’s Global Surveillance and Monitoring System, which collects safety data from over 100 countries. If you’re unsure, ask your pharmacist to check international databases. Never ignore a recall notice, even if your drug looks the same.