22 Dec 2025 |
Health
|
by
Brian Halstead

When you write a prescription, you’re not just choosing a medicine-you’re choosing a system. The shift from brand names to generic prescribing isn’t just about saving money. It’s about standardizing care, reducing errors, and making treatment accessible. In the UK, nearly 90% of prescriptions are now written using the International Non-proprietary Name (INN)-the generic name of the active ingredient. That’s not random. It’s policy. And it’s backed by decades of evidence.
Why Generic Prescribing Is the Default
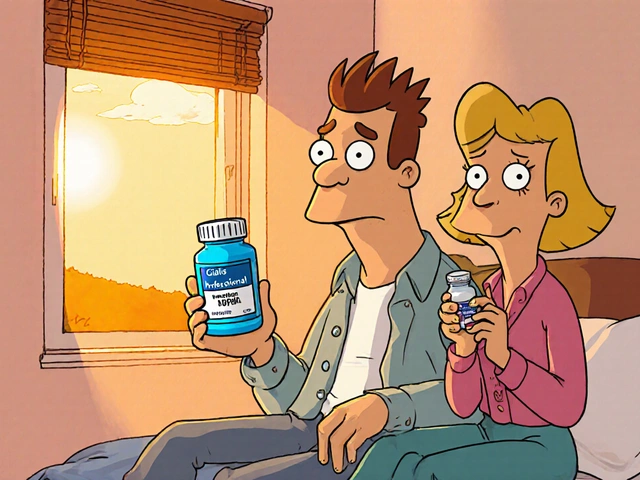
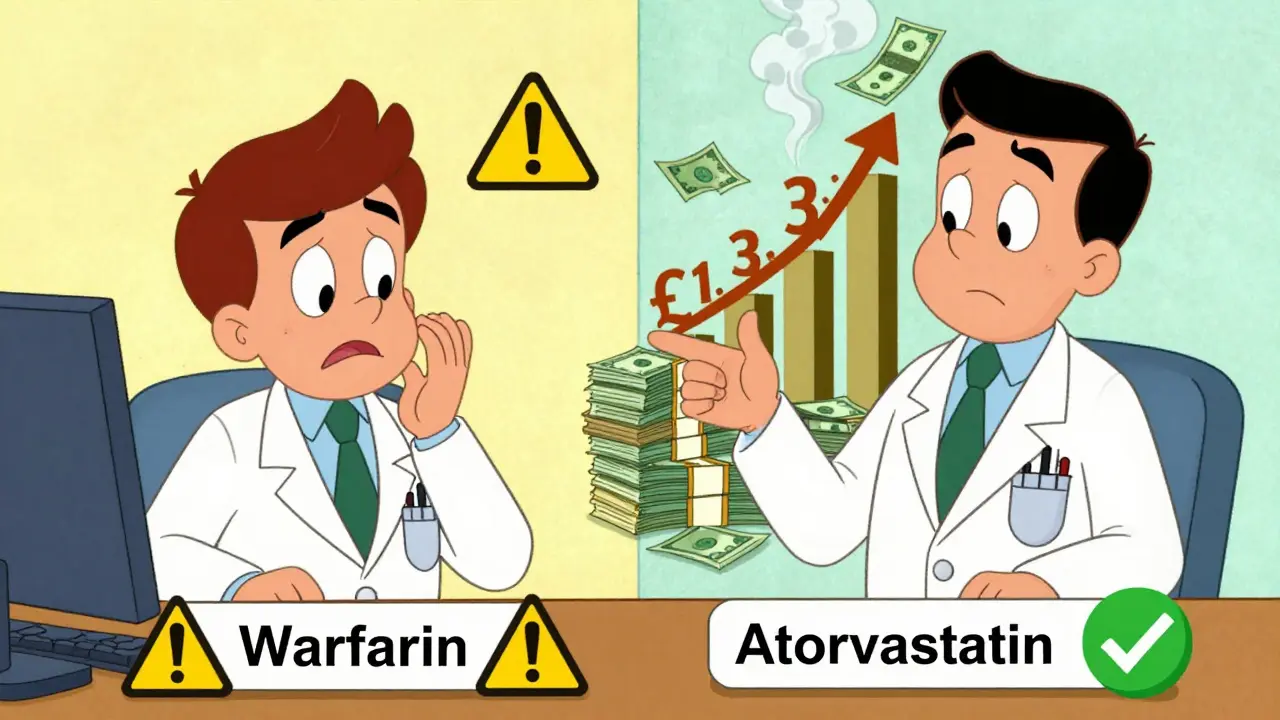
Generic drugs contain the exact same active ingredient as their brand-name counterparts. They’re required to meet the same standards for purity, strength, and performance. The difference? Price. Atorvastatin, the generic version of Lipitor, costs about £2.50 a month. The brand version? Around £30. Omeprazole, the generic for Losec, is £1.80 versus £15. That’s an 80-85% drop in cost. Across the NHS, that adds up to £1.3 billion saved every year. But it’s not just about savings. Generic prescribing reduces medication errors. Think about it: one drug, one name. No confusing brand variations like Prilosec, Losec, Omeprazol, or Omez. Just omeprazole. The Institute for Safe Medication Practices found that using generic names cuts prescribing errors by half. Fewer mix-ups. Fewer hospital admissions. Better outcomes. Patients also stick with their meds longer when they’re cheaper. A 2017 JAMA study showed that switching to generics improved adherence by 8-12%. That translates to 15% fewer hospitalizations for chronic conditions like high blood pressure or diabetes. When patients can afford their pills, they take them.When Brand-Name Prescribing Is Necessary
Generic prescribing isn’t a one-size-fits-all rule. There are exceptions-and they’re well-defined. The British National Formulary (BNF) and NHS England identify three categories where brand-name prescribing should be the norm:- Category 1: Narrow therapeutic index drugs-where small changes in blood levels can cause serious harm. These include carbamazepine, phenytoin, levothyroxine, digoxin, and warfarin. Even minor differences in absorption between generic versions can affect INR levels or seizure control.
- Category 2: Modified-release formulations-like theophylline or certain slow-release opioids. The way the drug is released over time matters. Some generic versions don’t replicate the release profile exactly, which can lead to under- or over-dosing.
- Category 3: Biologics and biosimilars-insulin, adalimumab, infliximab, and others. The MHRA explicitly states these must be prescribed by brand name. Why? Because even tiny changes in manufacturing can trigger immune reactions. Switching between biosimilars and originators isn’t risk-free.
What the Evidence Says About Safety
Some clinicians worry about switching patients from brand to generic. Especially in epilepsy. A 2018 meta-analysis in Epilepsia found a 1.5-2.3% higher rate of breakthrough seizures when patients were switched between different generic versions of antiepileptic drugs. That’s small, but it matters for someone who’s been seizure-free for years. The American Epilepsy Society recommends avoiding multiple switches in these patients. One switch, if necessary, is fine. But don’t keep swapping generics back and forth. Consistency matters. For levothyroxine, patient reports of fatigue or weight gain after switching are common. But studies show most of this is the nocebo effect-the opposite of placebo. When patients believe generics are inferior, they feel worse. A 2021 study found that when doctors explained the science-“This has the same active ingredient, same dose, same safety record”-patient acceptance jumped from 67% to 89%. Pharmacists report issues too, especially with modified-release tablets. One formulation might release the drug over 12 hours. Another might do it in 8. The patient doesn’t notice until they feel shaky or nauseous. That’s why electronic prescribing systems now flag these exceptions automatically.
How to Implement This in Practice
NHS England’s Generic Prescribing Toolkit gives a clear four-step plan:- Audit your prescribing-use the Prescribing Analytics Dashboard. See what percentage of your scripts are generic. Most GPs are at 92%, but some still lag.
- Learn the exceptions-keep the BNF’s three categories handy. Print them. Put them on your screen. Don’t rely on memory.
- Set defaults in your e-prescribing system-make sure the system auto-fills the generic name. Only override when necessary.
- Monitor and review-check your prescribing data every quarter. Are you hitting 90%? Are there spikes in complaints?