When your hands feel clumsy, your balance starts to slip, or you drop things you’ve held for years without issue, it’s easy to blame aging. But these aren’t just normal signs of getting older-they could be early warnings of cervical myelopathy, a serious condition where the spinal cord in your neck gets squeezed. It’s not just a stiff neck. It’s your nervous system sending distress signals. And if ignored, it can lead to permanent weakness, loss of coordination, or even paralysis.
What Exactly Is Cervical Myelopathy?
Cervical myelopathy isn’t just spinal stenosis. That’s a common mistake. Spinal stenosis means the space in your neck spine has narrowed-like a tunnel getting tighter. But myelopathy means that narrowing is actually hurting the spinal cord inside. Think of it this way: stenosis is the narrowing. Myelopathy is the damage caused by it. Most cases-about 75%-are called cervical spondylotic myelopathy (CSM). This happens slowly over time as your neck bones, discs, and ligaments wear down. Discs lose water and flatten. Bone spurs grow. Ligaments thicken. All of it pushes into the spinal canal. By age 70, nearly 1 in 10 people have this condition, even if they don’t know it yet. The spinal cord is like a high-speed cable carrying signals from your brain to your body. When it’s compressed, those signals get scrambled. That’s why symptoms show up in your hands, legs, and even bladder control-not just your neck.Early Warning Signs You Can’t Ignore
The earliest signs are subtle. People often brush them off. But here’s what to watch for:- Hand clumsiness-buttoning shirts, writing, or using keys becomes harder
- Feeling like your feet are “walking on cotton” or unsteady
- Weakness in arms or legs, especially when lifting or climbing stairs
- Increased reflexes in knees and ankles-your doctor can check this
- Numbness or tingling in fingers, arms, or shoulders
- Loss of fine motor skills-dropping pens, fumbling with zippers
How Doctors Diagnose It
A simple X-ray won’t cut it. You need an MRI. That’s the gold standard. It shows not just the narrowing, but also whether the spinal cord itself is damaged. Look for bright spots on T2-weighted images-that’s a sign of cord injury, not just compression. Doctors also use the Japanese Orthopaedic Association (JOA) score. It’s a 17-point test that checks movement, sensation, and bladder control. A score below 14 means you have myelopathy. This isn’t just paperwork-it guides whether you need surgery. CT scans and EMG tests help too. CT shows bone detail, and EMG checks nerve signals. But neither replaces the MRI. And don’t be fooled if your X-ray looks “fine.” Many people with severe myelopathy have normal-looking X-rays because the damage is inside the soft tissue, not just the bone. The average time to diagnosis? Over 14 months. Nearly half of patients see three or more doctors before getting the right answer. That delay costs you recovery potential.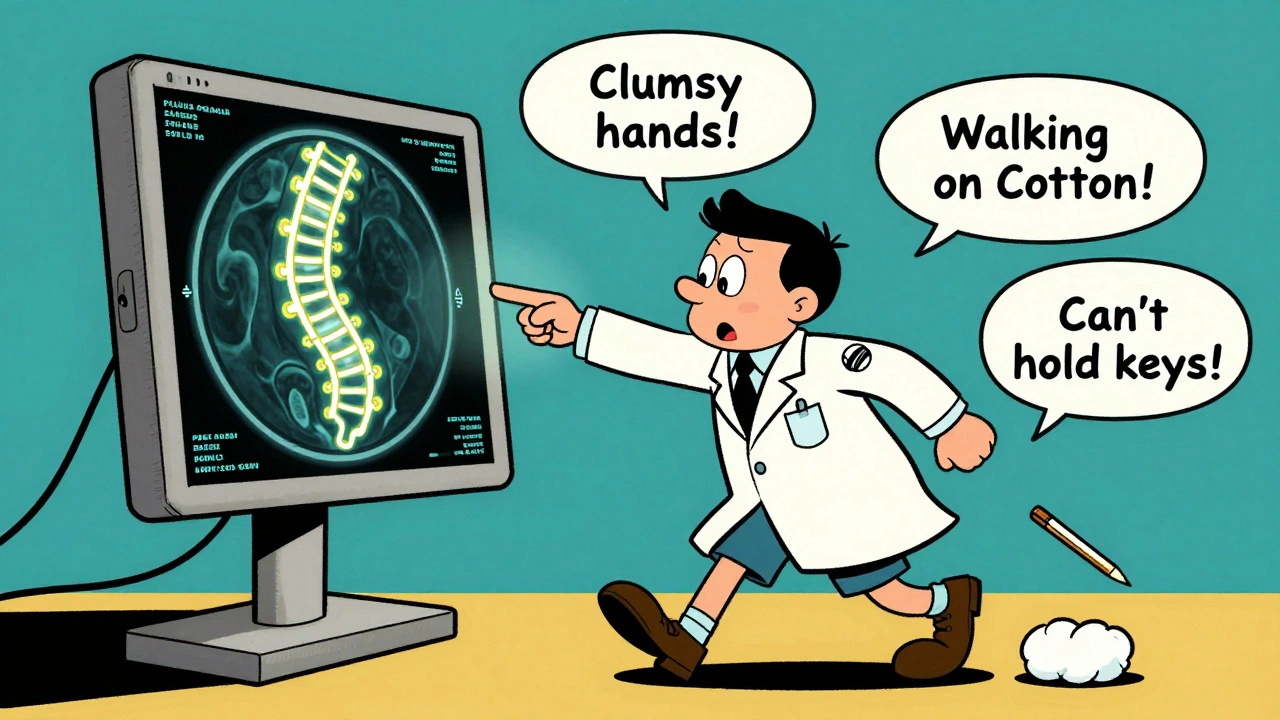
When Surgery Is the Only Real Option
Conservative treatment-physical therapy, NSAIDs, rest-might help a little. But studies show only 28% of mild cases improve over two years. Meanwhile, 63% get worse. If your JOA score is below 12, or if symptoms are getting worse fast, surgery is strongly recommended. The American Academy of Orthopaedic Surgeons gives this a Grade A recommendation-meaning the evidence is solid. There are three main types of surgery:- Anterior Cervical Discectomy and Fusion (ACDF): Removes the damaged disc from the front, fuses the bones. Best for single-level problems. Success rate: 85-90% for symptom relief.
- Laminectomy with Fusion: Removes the back part of the vertebrae and fuses the spine. Used for multi-level compression. Higher success for nerve recovery, but more neck pain afterward.
- Laminoplasty: Opens the back of the spine like a door instead of removing it. Preserves motion. Better for multiple levels. Less neck pain, but slightly lower nerve recovery than fusion.
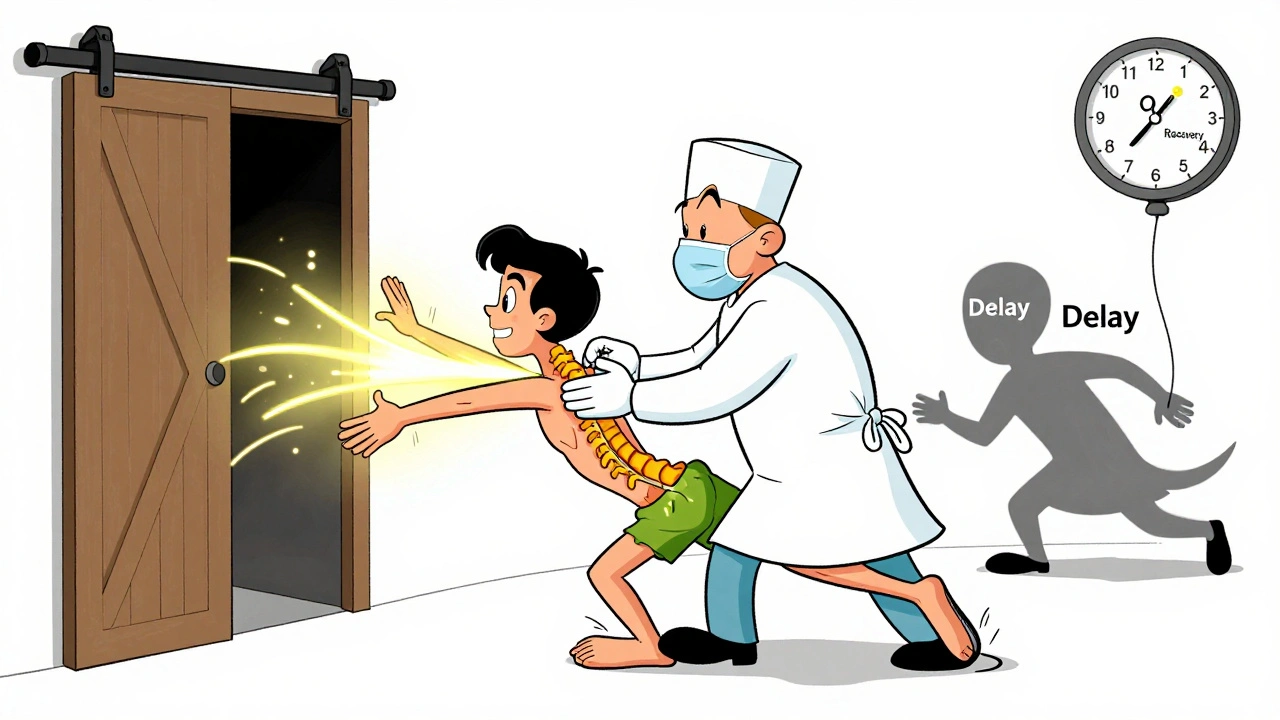
Timing Matters More Than You Think
This is critical: the sooner you operate, the better you recover. Patients who have surgery within six months of symptoms start show 37% better functional recovery than those who wait over a year. For every month you delay, your chance of full recovery drops by about 3%. Why? Because spinal cord damage isn’t always reversible. Once nerve cells die, they don’t come back. Early surgery stops the pressure before permanent harm sets in. A 2023 study at Emory Healthcare showed patients treated early were 2.7 times more likely to report “excellent” outcomes on the JOA scale. That’s not a small difference-it’s life-changing.What to Expect After Surgery
Hospital stay: 1-2 days for front surgery, 2-3 days for back surgery. Most people walk the day after. Recovery takes 3-6 months. You’ll need formal physical therapy for 8-12 weeks. Focus? Cervical stability, balance training, and regaining hand coordination. Common side effects:- Temporary trouble swallowing (22% after ACDF)
- Neck pain lasting 6 months (35% after fusion)
- Post-laminectomy syndrome: chronic neck pain (18% after posterior surgery)
Who Should Avoid Surgery?
Not everyone needs it. If your symptoms are mild, stable, and your MRI shows no cord signal change, watchful waiting might be okay. But you need regular check-ups-every 6 months. People with severe heart disease, uncontrolled diabetes, or who smoke are higher risk. Quitting smoking before surgery cuts fusion failure risk by half. Keeping blood sugar under control (HbA1c under 7.0) cuts infection risk from 8.5% to 3.2%. And here’s the hard truth: 15-20% of cervical spine surgeries today might be unnecessary. Too many are done without clear signs of spinal cord damage. That’s why doctors now use strict criteria-objective neurological loss, not just pain.What’s New in 2025?
Robotic-assisted surgery is becoming standard for complex cases. It improves precision and reduces revision rates from 10% to under 7%. Clinical trials are testing drugs like riluzole to protect nerves during surgery. Early results show 12% greater improvement in hand function at six months. Genetic markers like COL9A2 polymorphisms are being studied to predict who’ll degenerate fastest. Soon, treatment may be personalized-not just based on symptoms, but your biology.What You Can Do Now
If you’re experiencing hand clumsiness, unsteady walking, or loss of fine motor skills:- See your doctor immediately-not next month, not after the holidays.
- Ask for an MRI of your cervical spine. Don’t settle for X-rays alone.
- If myelopathy is confirmed, consult a spine specialist within two weeks.
- If surgery is recommended, don’t delay. Time is your biggest enemy.
Don’t wait until you can’t button your shirt. Don’t wait until you need a cane. Your spinal cord can’t wait.
Can cervical myelopathy get better without surgery?
In rare cases, mild cervical myelopathy with no progression may stabilize without surgery, but it won’t improve significantly. Studies show only 28% of mild cases get better over two years with conservative care, while 63% get worse. Waiting too long risks permanent nerve damage. Surgery is the only proven way to stop progression and restore function.
How long does recovery take after cervical myelopathy surgery?
Most people can walk the day after surgery. Full recovery takes 3 to 6 months. Physical therapy usually lasts 8 to 12 weeks, focusing on balance, strength, and hand coordination. Nerve recovery is slow-improvements can continue for up to a year, especially if surgery was done early.
What’s the difference between ACDF and laminoplasty?
ACDF is done from the front of the neck and removes a damaged disc, then fuses the bones. It’s best for one or two levels. Laminoplasty is done from the back and opens the spinal canal like a door, preserving motion. It’s better for three or more levels and causes less neck pain, but may have slightly lower nerve recovery rates than fusion.
Is cervical disc replacement better than fusion?
For eligible patients, disc replacement preserves neck motion and reduces stress on nearby levels, lowering the chance of future surgery. The M6-C implant, approved for two to three levels in 2023, shows 81% success in maintaining motion at 24 months, compared to 63% with fusion. But fusion still has higher long-term success in nerve recovery for severe cases.
Can I still walk or drive after cervical myelopathy surgery?
Most patients walk the same day or next day after surgery. Driving is usually allowed after 2-4 weeks, once neck movement is comfortable and pain is controlled. Full return to normal activities, including sports or heavy lifting, takes 3-6 months. Balance and coordination improve gradually with therapy.
Why do some people still have pain after surgery?
Some patients have lingering neck pain due to scar tissue, muscle stiffness, or adjacent segment stress. About 35% of ACDF patients report neck pain at six months. Post-laminectomy syndrome affects 18% of those with posterior surgery. These issues often improve with physical therapy and time. Persistent pain may need further evaluation, but it’s not always a sign of failed surgery.
What happens if I delay surgery too long?
Every month of delay reduces your chance of full recovery by about 3%. After 12 months, nerve damage becomes harder to reverse. Many patients who wait end up with permanent weakness, difficulty walking, or loss of bladder control-even after surgery. Early intervention is the single biggest factor in long-term outcomes.