Allergy Emergency Decision Tool
Emergency Decision Guide
This tool helps you quickly determine if epinephrine is needed based on symptoms and weight. Always act immediately if anaphylaxis is suspected.
Critical Anaphylaxis Symptoms
What an Allergy Action Plan Really Does
An allergy action plan isn’t just a piece of paper. It’s your lifeline during a reaction. When your body overreacts to something harmless-like peanuts, bee stings, or shellfish-it can shut down breathing, drop blood pressure, or cause swelling that blocks your airway. That’s anaphylaxis, and it doesn’t wait. A written plan tells you, your family, teachers, or coworkers exactly what to do before panic sets in. Studies show people with a plan use epinephrine 68% more often and end up in the hospital 42% less than those without one.
The One Medication You Must Always Carry
Epinephrine is the only medication that can stop anaphylaxis in its tracks. Antihistamines like Benadryl won’t cut it. They help with itching or hives, but they can’t open a swollen airway or raise a dropping blood pressure. Epinephrine does both. It’s not optional. If you or your child has a history of severe allergies, you need at least two epinephrine auto-injectors with you at all times-school, trips, restaurants, even the park.
Dosing depends on weight:
- 0.10 mg for kids 16.5-28.7 lbs
- 0.15 mg for kids 28.7-55.1 lbs
- 0.30 mg for anyone over 55.1 lbs
These aren’t guesses. They’re based on clinical guidelines from the American Academy of Pediatrics and the Asthma and Allergy Foundation of America. Using the wrong dose can be dangerous-too little won’t work, too much can cause heart problems. Always check your injector’s label. If you’re unsure, ask your allergist. And never, ever skip carrying a second one. Reactions can come back hours later, and you might need another shot.
When to Use Epinephrine-No Waiting
You don’t need to wait for symptoms to get worse. If you’ve been exposed to a known allergen and notice even one sign of a serious reaction, use epinephrine right away. The old rule-wait for two systems to be involved-is outdated. Experts now say: if you’re unsure, inject.
Signs to act on:
- Swelling of the tongue, lips, or throat
- Wheezing, trouble breathing, or tightness in the chest
- Dizziness, fainting, or confusion
- Vomiting or diarrhea after eating a trigger food
- In babies: sudden hives, limpness, or a high-pitched cry
For people with asthma or past anaphylaxis, the risk is even higher. One study found these individuals are three times more likely to have a life-threatening reaction. If you’re in that group, your plan should say: inject at the first sign-even if it’s just a few hives after eating peanuts. Delaying epinephrine by just 10 minutes can cut your survival odds in half.

What About Antihistamines and Inhalers?
Antihistamines like diphenhydramine (Benadryl) have a role, but only as a second step. Use them only after epinephrine, or for mild reactions with no breathing or blood pressure issues-like a few hives with no other symptoms. Never use them instead of epinephrine. A 2021 study found that in schools, giving Benadryl first delayed epinephrine by an average of 22 minutes. That delay cost lives.
For people with asthma who have allergic reactions, an albuterol inhaler helps if they start wheezing. But again, epinephrine comes first. If you’re wheezing and have a known allergen exposure, inject epinephrine, then use your inhaler. Don’t wait to see if the inhaler fixes it. The airway swelling from anaphylaxis won’t respond to an inhaler alone.
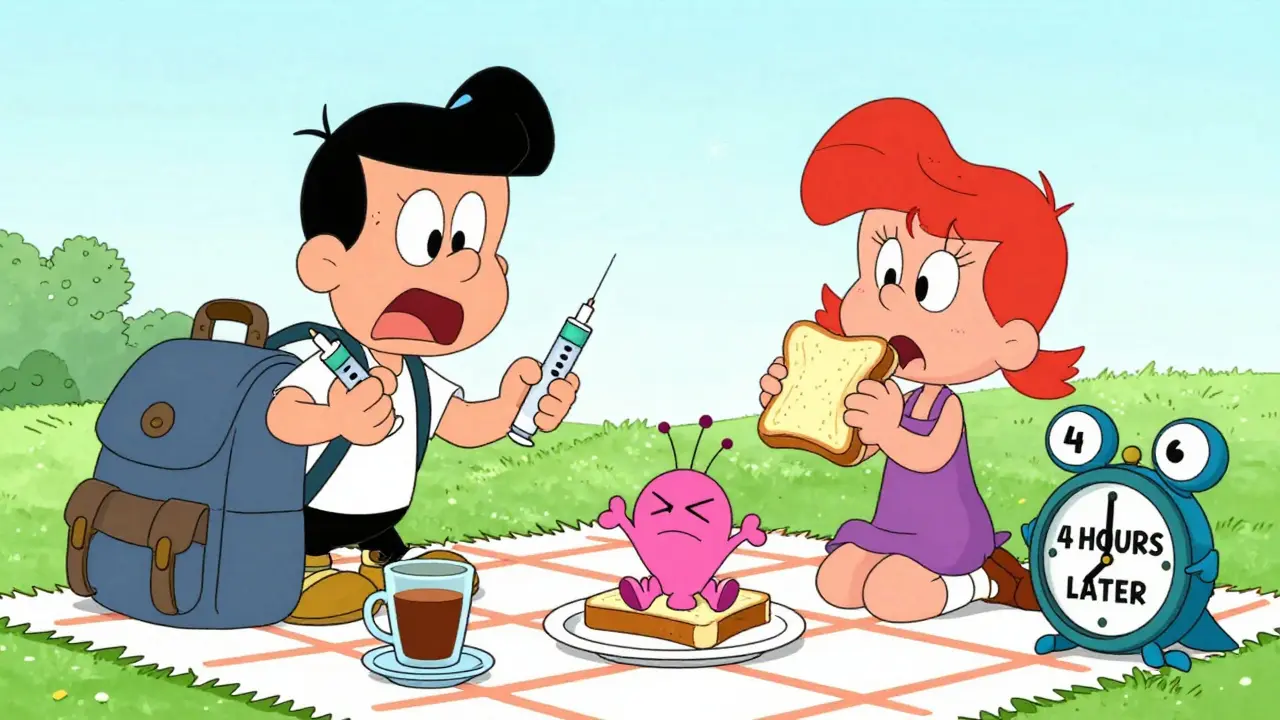
What Happens After You Inject
Injecting epinephrine isn’t the end. It’s the start of emergency care. Even if you feel better, you must go to the hospital. About 20% of people have a second wave of symptoms hours later-called a biphasic reaction. This can happen even if you thought the first one was over. You need to be watched for 4 to 6 hours. Paramedics or ER staff will monitor your heart, blood pressure, and breathing.
Don’t assume you’re safe just because the shot worked. That’s when people make fatal mistakes. If symptoms return or worsen after the first shot, give a second dose of epinephrine. Wait at least 10 minutes between doses. Most auto-injectors come with two doses for exactly this reason. Keep the used injector with you when you go to the hospital. They’ll need to know what you took and when.
Common Mistakes and How to Avoid Them
Most allergy-related deaths happen because epinephrine wasn’t used in time. Here are the top mistakes-and how to fix them:
- Expired injectors: Check expiration dates every month. Epinephrine loses potency over time. Replace them before they expire. Keep a spare in your bag, car, and workplace.
- Not carrying two: One isn’t enough. Reactions can come back. A second dose may be needed. Keep one at school, one at home, and one with you.
- Waiting for symptoms to get worse: If you’re exposed and feel even slightly off, inject. Don’t wait for throat swelling or vomiting.
- Confusing symptoms: Hives alone? Maybe just a mild reaction. Hives + vomiting? That’s anaphylaxis. Use your plan’s symptom checklist. If you’re unsure, treat it as severe.
- Not training others: Teachers, babysitters, coworkers-they need to know how to use the injector. Practice with a trainer pen. Show them where to inject (outer thigh, through clothing if needed).
Digital Plans and New Options
More people are using digital versions of their allergy action plans. FARE’s app, launched in early 2024, lets you store your plan, set reminders for injector replacements, and share emergency contacts with one tap. Over 140,000 people use it. Some newer injectors even have Bluetooth that connects to your phone to log when you used it.
There’s also a new option: Neffy, an intranasal epinephrine spray approved by the FDA in 2023. It’s easier for people who hate needles. But it’s not for everyone. It doesn’t work as fast as an injection for severe cases. Talk to your doctor before switching. Most plans still recommend injectable epinephrine as the gold standard.
Getting a Plan That Works
Your doctor should give you a personalized plan right after your allergy diagnosis. But only 58% of patients actually get one completed. If yours is missing, ask for it. Use templates from the Asthma and Allergy Foundation of America or Food Allergy Research & Education. Fill out the form with your allergist-include your exact triggers, dosing, and emergency contacts. Sign and date it. Keep a copy in your wallet, your child’s backpack, and your phone.
Share it with schools, daycare centers, and camps. Most states require schools to have individual health plans for kids with allergies. If they refuse, remind them: it’s the law. And if your plan is outdated, update it every year-or after any major reaction.
Final Thought: Confidence Comes From Preparation
Living with severe allergies is scary. But you’re not powerless. A clear, updated action plan gives you control. It turns fear into action. You don’t need to be a medical expert-you just need to know what to do, and when. Carry your epinephrine. Know the signs. Use it early. And never, ever doubt your instincts. If something feels wrong, act. Your life depends on it.
Can I use Benadryl instead of epinephrine for a severe reaction?
No. Benadryl only treats mild symptoms like itching or hives. It cannot stop airway swelling, low blood pressure, or shock-any of which can be fatal. Epinephrine is the only medication proven to reverse anaphylaxis. Delaying it to give Benadryl first increases the risk of death.
How do I know if I need two epinephrine injectors?
If you’ve ever had a severe reaction, have asthma, or your allergist says you’re at high risk, you need two. About 20% of reactions come back hours later. One injector might not be enough. Always carry two, even if you think you’re fine. It’s not overkill-it’s standard care.
What if I’m not sure whether it’s a reaction or just feeling sick?
If you’ve been exposed to your known allergen and feel unusual-dizzy, short of breath, nauseous, or breaking out in hives-inject epinephrine. It’s safer to use it when you don’t need it than to wait and regret it. Epinephrine is very safe for most people. Side effects like a racing heart are temporary. Not acting can be deadly.
Do I still need to go to the ER after using epinephrine?
Yes. Even if you feel fine after the shot, you must go to the emergency room. About 1 in 5 people have a second wave of symptoms hours later. This is called a biphasic reaction. Medical staff need to monitor you for 4 to 6 hours to make sure it doesn’t come back.
Can I reuse an epinephrine injector?
No. Epinephrine auto-injectors are single-use devices. Once activated, the needle locks and the medicine is gone. Even if it looks like there’s liquid left, you can’t safely reuse it. Always replace it after use. Keep a spare ready at all times.
Are there alternatives to injections?
Yes-Neffy is an FDA-approved nasal spray that delivers epinephrine. It’s easier for needle-averse users and children. But it’s not as fast or reliable as an injection for severe reactions. It’s an option, not a replacement. Talk to your allergist to see if it’s right for you. Most experts still recommend injectable epinephrine as the first choice.